Antibiotic resistance is spotty. If you are hospitalized in New York and you acquire a Gram-negative infection in the hospital, there is a reasonable chance it will be caused by a highly resistant pathogen. If you go to a hospital in New Hampshire or Vermont, there is almost no chance for that to happen. ACSH advisor Dr. David Shlaes explains.
MRSA
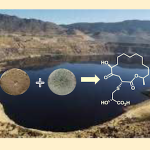
University of Montana researchers discovered that when grown in co-culture, two different species of the fungus Penicillium – the same genus that produces the antibiotic penicillin – cooperate to synthesize an antibiotic that neither species produces when grown alone.
You never know when you're going to find yourself 2,067 feet underwater off the coast of the Bahamas, looking for a sponge that doesn't exist yet. It's just another day at the office for antibiotic research scientists.
The Antarctic sea sponge, Dendrilla membranosa, may provide an answer to fighting MRSA, or methicillin-resistant staphylococcal infections. A Florida university research team has identified a sponge extract, which it named darwinolide, that in a laboratory was able to prevent 98 percent of MRSA growth.
A British microbiologist found that some beard bacteria contains anti-adhesion molecules, which prevent bacterial binding to surfaces. That means that hipster beards may harbor bacteria capable of killing drug-resistant bacteria.
According to a recent report from the British Broadcasting Corporation (BBC), experts are questioning the utility of current hospital practices designed to fight the spread of MRSA methicillin-resistant Staphlococcus aureus, also known as a superbug .
We at ACSH have written frequently about the misguided change in mindset by the FDA two decades ago that brought most antibiotic research to a dead stop.
No one has been deeper in the FDA trenches than ACSH advisor and infectious disease expert Dr. David Shlaes. He has been blogging, advising, lobbying, begging, and doing just about everything short of pulling his hair out to convince the infectious disease division of the FDA to reverse the disastrous changes in clinical trial policy that caused almost all drug companies to abandon research in this area.
The emergence of antibiotic-resistant bacteria, in particular a strain of Staphlococcus aureus (SA ) resistant to methicillin (MRSA) (a member of the fluoroquinolone class of drugs) has concerned physicians and caused hospitals to review and revamp their sanitation procedures.
We at ACSH have warned repeatedly about the nightmarish scenario that continues to unfold as more and more bacteria become resistant to previously-effective antibiotics, bringing us to the precipice of the pre-penicillin era where common infections such as strep throat and pneumonia were killers.
ACSH advisor Dr. David Shlaes, a world-renowned expert on antibiotics and the bacteria that are increasingly resistant to them, encourages all of us to watch Frontline tonight at 10 EST. They are covering a topic that you
It may sounds counterintuitive, but a study just published online by JAMA concludes that the use of gloves and gowns by health care workers in intensive care units (ICU)
Antibiotic resistance is a serious and persistent national problem. For example, Staphlococcus aureus bacteria that are resistant to the antibiotic methicillin (MRSA) have become common throughout the US, causing invasive infections of skin and soft tissues as well as bloodstream infections in patients in critical care settings.