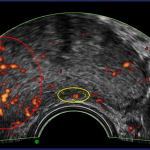
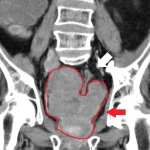
Have you ever felt like you're just waiting for the other shoe to drop, especially regarding medical test results? Francis Collins, former NIH director, found himself in that situation, dancing the delicate tango of active surveillance for prostate cancer. Imagine a urine test that could cut down on those nerve-wracking biopsies while boasting a 99% accuracy rate for spotting the serious stuff.
prostate cancer
Given the low mortality from slow-growing, localized prostate cancers and the side effects of many treatments, deciding whether to opt for monitoring or treatment can be excruciatingly difficult.
Medicine, like the science that underlies it, is seldom transformed by “Eureka” breakthroughs; rather, it is most often a process of systematically accumulating knowledge and making incremental advances. Radiation treatment for breast cancer is a good example: New data has enabled us to revise and improve old approaches.
Medicine aims to identify social determinants of health (SODH) and level the playing field of outcomes so that we all receive equitable care. But measuring disparities is not as easy as it might seem. A meta-analysis of prostate surgery suggests more equality than disparity.
Editors at the journal Nature Medicine recently asked researchers and public health experts from around the world to identify clinical trials that will shape medicine in 2023. They came up with a varied list of candidates, from cervical and prostate cancer screening protocols to gene therapy for muscular dystrophy and new drugs for Parkinson’s disease and Alzheimer’s disease. The selections are arbitrary and idiosyncratic, but they are interesting, nevertheless.
“Compared with white men, African American men are more likely to develop prostate cancer and are twice as likely to die from the disease.” National Cancer Institute [1]
The underlying “reasons” are biological, cultural, and societal. A new JAMA Oncology study looks at societal causes.
My PSA was 22 – but my biopsy only showed inflammation. I was needlessly upset, and it seems like I underwent an unnecessary procedure. There has to be a better way!
Amazing, recent progress in prostate cancer research has encouraged many experts (including this writer) to expect that this type of cancer will be cured -- or at least adequately controlled -- within their lifetimes. "I’m glad I had this cancer," states Dr. Paul Lange, "for it made me a more empathetic physician."
Controversy abounds in prostate cancer. It can involve who and when to screen, and which treatment is the best. A recent study looks at what's been less controversial: the adjunctive use of androgen deprivation therapy. It appears to increase the risk of dementia.
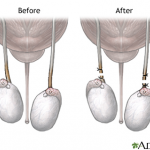
One very sure means of contraception is vasectomy — a minor surgical operation that blocks the transfer of sperm from a man's testes to his urethra (and thus to his partner) by interrupting the tube leading from the testis. One concern has been that somehow this procedure might increase the risk of prostate cancer. But now a meta analysis has found that the risk is virtually non-existent.
A new paper published in the journal Open Forum Infectious Diseases showed that 3 percent of men who undergo prostate biopsies end up being hospitalized within a month. Worse, half of those hospitalizations are due to an infection – and 45 patients died.
The U.S. Prevention Services Task Force released its 2017 draft recommendations for prostate cancer screening. Here we extensively address the new guidelines, clarify the role of the PSA test, and delve deeper into the topic with Dr. David Samadi, Chairman of Urology and Chief of Robotic Surgery at New York's Lenox Hill Hospital.