Should you be unfortunate enough to suffer from asthma, things are looking up. There are new biological therapies out there that "attack" asthma in novel ways. They are effective and are badly needed. The impact of the disease on people afflicted with it is probably more severe than you think. It's not as simple as carrying an inhaler around.
People with moderate-to-severe asthma have to endure far more than that. I know this. I am one of them.
The following statistics (annual, US only) may be eye-opening.
- 4,000 deaths
- 11 million attacks
- 2 million emergency room visits (more than 25% of all ER visits)
- 365 thousand hospital admissions
- The annual cost of asthma is $18 billion
Before 2003, common therapeutic options included rescue inhalers, inhaled steroids (1), oral bronchodilators, and various drugs that countered inflammatory components of the immune system. But about 5-10% of asthmatics don't respond to these treatments, so the only remaining option is prednisone, which is not something you want to take unless absolutely necessary (See: Prednisone: Satan's Little Helper).
Each of these therapies had drawbacks. Better methods to address the root causes of asthma were needed and they came to us in the form of injectable proteins and antibodies. As with all biologics (2), these drugs had to be given by injection (or IV), were quite expensive (3), and carried a small risk of severe immunological side effects (4). But they work quite well, and I have little doubt that these drugs will be the cornerstone of severe asthma in the future. Let's look at them.
Xolair (omalizumab, 2003)
Xolair was the first biological drug approved for moderate-to-severe asthma. It has a unique mechanism of action: binding to IgE, the "allergic antibodies" in our blood. People who have high IgE levels are allergic. And guess what? It's time for a QUIZ where you can win a BADASS ACSH COFFEE MUG if you're the first person to give the right answer.

QUIZ: High IgE levels cause misery for those of us who are plagued with too many of the antibodies. But they are not in our blood us by accident. What is the evolutionary adaptive advantage of having a high level of IgE? (Don't even think about Wikipedia. I'll know and will send you my shorts instead.)
Xolair (omalizumab, 2003), which is typically given twice per month by injection, is indicated for asthmatics with IgE levels between a certain range, "sops up" some of the IgE, thus decreasing the magnitude of the immune system associated with high levels. And it works pretty well. In adults and children who had poorly controlled asthma, it reduced clinically significant asthma exacerbations by 26-33%. A Cochrane review concluded that the drug reduced asthma symptoms, and was useful in helping some people discontinue orally inhaled steroids, but not with severe asthmatics who were on both omalizumab and steroids.

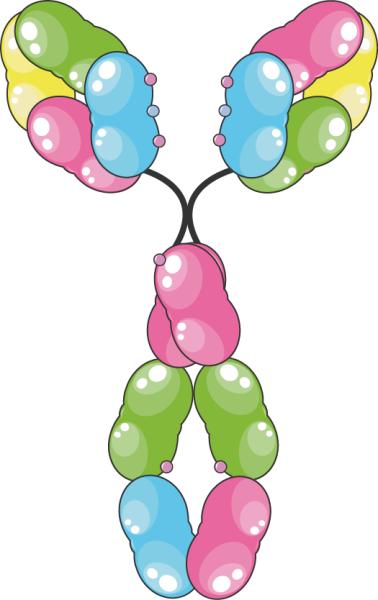
A graphical representation of the IgE antibody. Photo: Server Medical Art
Anti-eosinophilic antibodies: Nucala (mepolizumab, 2015)Cinqair (reslizumab, 2016),
Cinqair and Nucala are monoclonal antibodies which operate by a mechanism which is different from that of Xolair. They are considered to be more "heavy hitters" than Xolair, and were designed to treat a different form of asthma called eosinophilic asthma - a severe form of the disease. The drugs operate by going after a different allergic target - Interleukin 5 (IL5), a cytokine (3). IL-5 is an immune system protein which activates the production of eosinophils a sub-type of white blood cells which are responsible for fighting off a variety of pathogens. But when too many eosinophils are released, the cells accumulate in tissues where they cause cell damage and inflammation by a number of mechanisms. Both drugs are given monthly; Cinqair by IV infusion and Nucala by injection. As with Xolair, life-threatening anaphylaxis is possible but rare. But how well do they work?Both drugs have been approved for severe eosinophilic asthma as add-on therapies, not replacements for them, and the evidence for their effectiveness is limited. A new Cochrane review about anti-eosinophilic monotherapy is less than glowing:
"There were small improvements in quality of life and breathing tests [in patients who took any of three anti-eosinophilic drugs], but these may be too small to be detected by patients. We agree with international guidelines that say that these treatments can be added to standard treatment for people with severe asthma. However, we think that further research is needed to clarify some aspects, such as how to assess treatment response and how long to give treatment for."
H. Farne, et. al., Mepolizumab, reslizumab or benralizumab for people already taking inhaled steroids and long-acting beta2-agonists for their asthma. September 2017
Dupixent (dupilumab) Two for the price of one?
Dupixent is not an approved asthma drug; it got the nod from the FDA earlier in 2017 for a different allergic response - eczema. People who are highly allergic often have a "triad" called atopic dermatitis: asthma, eczema, hay fever, which typically occur together. (Atopic means that the eczema is not coming from the skin (e.g., contact dermatitis), but rather, internally.) So, why is it here? Because Dupixent also works against asthma, and, apparently quite well.
It reduced the frequency of severe asthma attacks by 46% in the group overall and by 60% to 67% in patients with high levels of eosinophilic cells. The trial involved 1,902 patients, including 1,795 adults and 107 adolescents. A September 11 press release by Regeneron and its partner Sanofi included some intriguing results.
A phase III clinical trial involving met both of its primary endpoints, the frequency of attacks, and a standard measure of lung function called (FEV1). The frequency of severe attacks was reduced by 46%, and by 60-67% (depending on the dose) in the sub-group of participants who had high levels of eosinophils. And the drug also improved FEV1 by 9-18%. The companies are hoping for FDA approval for asthma in 2018.
In summary, the current asthma biological drugs have been shown to work, but (usually) not well enough to replace current therapies. But keep in mind that the first drugs for a new disease or infection rarely turn out to be the best. Inverase (HIV) and Victrelis (hepatitis C) were the first direct antiviral drugs to be approved. Second-and-third generation drugs (ignorantly named "me too" drugs) were far better and blew by them immediately. Neither is used today.
So, I think the future is very bright for immune-based biological therapies for asthma, but we are not there quite yet. Other companies are developing similar drugs, and with a little luck, perhaps we will all breathe a little easier.
Notes:
(1) Inhaled steroids have typically been combined with long-acting beta agonists (LABAs), which are slow-acting bronchodilators. But LABAs have their own baggage. They not only do not work on their own but in the absence of the steroid component LABAs have led to increased deaths. Nor do LABAs have any use in treating acute asthma attacks.
2) Biologics are very different from small molecule drugs (pills). Although they are both drugs, biologics are large molecules, usually proteins, which must be given by injection. They cannot survive the conditions in the stomach because they are rapidly degraded. Biologics are also more difficult to make and purify than traditional drugs. This is one of the reasons for their high cost.
(3) Both Genentech (Xolair) and Teva (Cinqair) have patient assistance programs, which reduce the co-pay from hundreds of dollars to $5 or less. I have qualified for both with no trouble.
(4) When starting Xolair, new patients are required to wait in the physicians' office for at least an hour for observation for the first few injections. They also much carry epi-pens at all times, even though the incidence of anaphylaxis is only 1 in 1,000.
(5) Cinqair is not approved for anyone younger than 18. There are not yet data that support its safety and efficacy in younger asthmatics.
(6) Disclaimer: My IRA portfolio contains a small amount of Regeneron stock. The American Council receives no money from Regeneron (although we would certainly like to) or any other drug or medical device company.