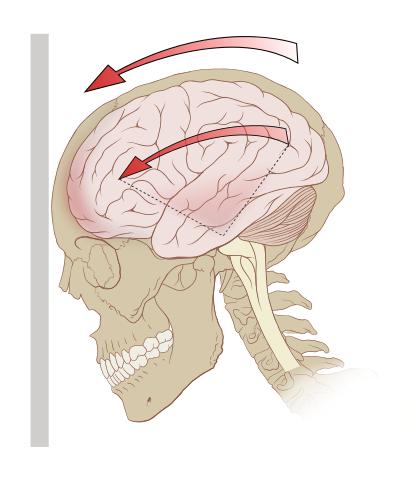
Concussion remains a problem for several reasons, not the least of which is that it is a clinical diagnosis, based on the symptoms reported to physicians. There are no objective physical findings to make the diagnosis; it is a diagnostic dilemma. Symptoms are non-specific and often do not correlate with objective measures of injury [1]. As a result, estimates of the incidence of concussion are subjective. In addition, according to the CDC nearly 500,000 children ages, 0-14 are seen in emergency departments for traumatic brain injury annually, and half of them are less than four years of age making symptom identification even more difficult, requiring reliance on the reports of very concerned parents. Without an evidence-based diagnosis, it is challenging to develop an evidence-based treatment.
A study by Jeremiah Johnson and his colleagues, Association of Salivary microRNA changes with prolonged concussion symptoms, published in JAMA Pediatrics attempts to establish an objective marker, microRNA (miRNA). These snippets of RNA influence the production of proteins and can be found in many fluids, including saliva making for a readily obtained, non-invasive biomarker. The study looked at the prognostic ability of miRNA versus standardized reporting of symptoms by both children and their parents [2]
52 children were seen within two weeks of a clinical diagnosis of concussion or mild traumatic brain injury (majority enrolled within the first week) and had their salivary microRNA measured on admission to the study, at 4weeks and eight weeks. The standardize reporting of symptoms was also obtained in those time frames. The object was to identify and predict acute concussion syndrome (ACS), which lasts less than a month, from prolonged concussion syndrome (PCS).
- There were no demographic, medical or concussion differences in the two groups, ACS and PCS
- 90% were Caucasian, 25% on non-steroidal anti-inflammatory drugs and 15% were taking a stimulant or selective serotonin uptake inhibitor for psychological symptoms (depression, sleeplessness and lack of concentration)
- 42% of concussions were from a sports-related injury, 15% from motor vehicle accidents, 46% had prior concussions
- 48% had symptoms of amnesia, and 27% had reported a loss of consciousness
The standardized report of symptoms was used to stratify the two groups into acute and prolonged. Initially, those children who developed PCS reported greater symptom severity but no difference in the number of symptoms as compared with children who only had ACS. Reporting by parents showed no differences in severity or number of symptoms for either cohort. By definition, children with PCS had higher symptom reports at four weeks, and these symptoms continued for at least eight weeks for 29% of the PCS cohort. miRNA was taken at each interval. Using retrospective analysis, the miRNA most sensitive in discriminating between ACS and PCS were identified as potential biomarkers. These miRNA were involved in signaling during synaptic development, neuronal migration, and repair, synapse strength, axon guidance, and development – all processes you might expect with repair after TBI.
miRNA changes were able to predict 85% of those children developing prolonged concussion syndrome as compared to standard symptom reporting by the children at 65%, by the parents at 56% and the regression model incorporating demographic and medical information of 63%. miRNA was more predictive.
But before getting too far ahead of ourselves, we should recognize the small size and retrospective nature of the study. We need to confirm miRNA’s predictive ability prospectively. The value of the work is that it may identify objective markers that physicians can use for diagnosis. More accurate diagnosis will result in more targeted therapy. At this time the treatment for ACS is rest, but for how long and are there other measures we can apply to hasten or improve recovery? In addition, more objective information may more quickly allay both the patient and their parent’s concerns. Hopefully, a prospective study is in the works, and we can begin to put our fears and treatment of concussion on a more objective footing.
[1] International Classification of Diseases-10 our standard for diagnosis defines prolonged concussion syndrome as having “3 or more of the following symptoms: headache, dizziness, fatigue, irritability, insomnia, concentration difficulty, or memory difficulty.”
[2] One standardize form was the Sports Concussion Assessment Tool (SCAT3), the other a similar test modified with patient history and demographics such as sex, age, previous concussion history, headache, fatigue, processing difficulty and migraine history