Both Dr. Wells and I often write, as clinicians, about the changing landscape in healthcare, bemoaning how administrators or technologies break the patient-physician relationship. But sometimes there is a self-inflicted wound when physicians for a variety of reasons move away from caring for patients to providing procedures. A presentation at the recent European Association of Percutaneous Cardiovascular Interventions is, unfortunately, a perfect example. (The inclusion of intervention in their title is the first clue that we may have a problem)
Stroke is a debilitating disease most frequently due to a blood clot blocking flow and oxygen to a part of the brain. There is a lot of effort made to reverse the effects of stroke in the first few hours before there is a loss of brain tissue, by removing the clot. The use of drugs to dissolve the clots helps some individuals, but the mechanical removal of the clot (thrombectomy) using a catheter may well help more patients return to normal function. The difficulty is that very few physicians in Europe, and the US, are trained in the techniques involved. The chair of this group of cardiologists provides the solution: “The equipment for mechanical thrombectomy is available; it's the trained specialists to perform the procedure that are lacking. This situation could be solved by training cardiologists to perform mechanical thrombectomy." All it would require is a three-month training course.
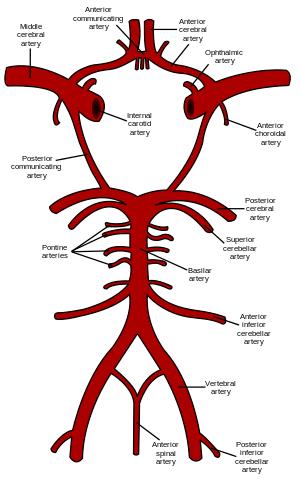
Typical training of neuroradiologists, specially trained in treating the blood vessels of the brain, requires two-years. The facile cardiologists already have experience with catheters, wires, stents, and drugs for the arteries of the heart and have, in some instances, already advanced their catheters into the main artery going to the brain to prevent strokes (carotid angioplasty), so why not?
I cannot argue that such an arrangement will increase the number of physicians able to treat this condition, but it will also lead to more bad clinical outcomes because highly skilled technique and judgment come not from a three-month training class, but from a dedication to a group of patients and the care they require. All arteries are not the same, in name, location and more importantly how they respond when manipulated. So the training of cardiologists is not entirely transferable. More importantly, is a three month training period enough to pass along judgment, or at least enough experience to do no harm? These techniques have a learning curve, but the learning curve for judgment is far longer, it is our clinical lifetime. [1]
Once the intervention is completed, who will care for the patient? This is a problem the cardiologists share with the neuroradiologists, but the latter have established teams to provide follow-up care and more importantly real-time peer-review of outcomes. Are the cardiologists planning on creating a program, with all that entails, dedicating a portion of their time to caring for these patients or is this another example of drive-by care? And will the volume of patients be sufficient to maintain the skill and judgment of cardiologists and their team?
Having the right physician in the right place at the right time for the right patient is a logistical nightmare than even Amazon cannot untangle. The offer by the cardiologists is a tradeoff; more care but provided by professionals with less training. I wonder if the cardiologists would feel the same way if a new breed of low-cost interventionalists, only trained in techniques, entered their clinical space? Or would they be the first to point out that caring for patients is more than just doing procedures? When you think about the “shortage” of physicians, this is a tradeoff we all must keep in mind.
[1] Factoid – the term a “steep learning curve” to describe an extended period of training is somewhat of a misnomer. The curve of learning over time, when steep, implies rapid acquisition of knowledge. A flatter curve, a lower rate of learning over time is what we really mean. That said, the metaphor works.