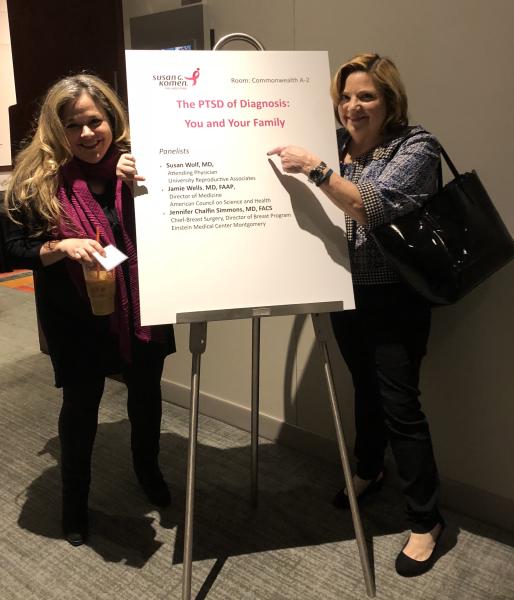
I had the distinct pleasure of presenting at Komen’s Pink, Purple Strength and Unity Conference on coping with a breast cancer diagnosis and how best to manage navigating such a trauma for you and your family. Topics discussed covered a wide range from optimal ways to communicate with your children (see here), partner, loved ones, doctors and care team to how to deal with new challenges to your sexuality and intimacy. It was an incredibly rewarding experience as the day was focused around education, sharing and support-building for breast cancer survivors and individuals living with metastatic breast cancer.
Here are some themes that can help with the trauma of diagnosis and moving forward
There is a reason on planes when going through safety instructions you are advised to put the oxygen mask on yourself before you can assist anyone else. The time it takes you is the time it takes you to equilibrate after the shock of such life-altering news. For some that is more rapid, and that is normal. For others that is more protracted, and that too is normal. There is no right path, just what is right for you. Most people in your life will take cues from you and your reaction, which can be burdensome at times and reverberate through families. Communicating early and often can be very helpful in assuaging fears and minimizing unnecessary additional stress.
How do you take care of yourself to take care of your family
A cancer diagnosis is disconcerting at best no matter where you fall on the continuum. Whether burdened with worry due to a strong family history and awaiting word on your biopsy, having developed breast cancer while pregnant or even after treatment while in remission, the weight of concern and fear can be overwhelming, sometimes debilitating. The stress of therapies, side effects, appointments and the all-consuming nature of chronic disease has an impact on the patient and their families that can often feel like too much to handle.
Where you are in your life cycle, albeit during your reproductive years or later in age, will play a meaningful role in the type of support you will need and what is required of your day-to-day. Identifying your medical needs as well as your individual, personal ones is a vital first step.
The good news is despite the many challenges you face there are tools that can ameliorate some of the anxiety you endure, allowing you to be more empowered in your journey. A shifting emphasis on controlling the controllable can yield significant dividends – not just for your mind, but your body and future as well.
The Gift of Resilience
Resilience is a tricky thing, routinely not tested until a person experiences extreme circumstances. But, it is a worthy ally; not only throughout a disease course’s winding path, but also in its influence on positive treatment outcomes. Depending on the study, it is estimated that between 20-25% (with research reporting upward of 50%) of patients with breast cancer meet the criteria for depression, up to 32.3% for post-traumatic stress disorder (PTSD) and upwards of 75% with symptoms not quite meeting the criteria for disorder. Such eventualities can impair prognosis. Once sustained in a chronic nature, PTSD is associated with noncompliance, and higher rates of spread and recurrence.
This is not an inevitable option and does not have to be your story. It is completely normal to feel a spectrum of emotions occupying a vicious cycle of good, not-so-good and bad days. You may go through periods of relating to and not relating to those closest to you. Feelings of guilt are common for interims of absence or diminished quality time with children or a spouse can foster great sadness and frustration.
Feel what you feel and move through the emotion. You can do yourself an invaluable service if you can channel some of that energy into finding strength in what is in front of you. The more you practice, like any exercise, the better you will get at forcibly stopping negative thoughts. Accepting that some things in life are outside of your control will allow you to let go of what isn’t serving you, so you can focus on strategies that can reduce your stress. By identifying what is most anxiety-provoking, you are winning half the battle in implementing methods to quell some of that toxicity. It is okay that some days might make this effort more realistic than others.
That said, many patients believe they need to be a superhero and be able to manage everything replete with a smile, which can impose more pressure in the process. If words like "battle" and "warrior" don't work for you, then don't use them. If they do, then embrace them. There is your way, not one right way to adjust to living with disease. Asking for help when the emotional component overwhelms is an invaluable step to coping and improving one’s stress. There are a number of support networks and avenues for relief when feeling this way and your health care team can guide you. And, they will do so happily.
The Harms Of Persistent High Stress
People process change and disappointment in varied ways — some take longer than others. Whoever moves through uncertain and volatile times more speedily with less pessimism is apparently best served. The physical well-being achieved is now backed by some encouraging data, for example:
An 11-year study in Finland researched factors that pose a risk of developing coronary heart disease (CHD). With increasing evidence connecting mental health and personality traits to CHD, this group investigated the influence of optimism and pessimism on mortality. They found:
-
Those who died from CHD were significantly more pessimistic at baseline than others.
-
The most pessimistic were 2.2-fold more likely to die than the least.
-
Optimism was inconclusive as a risk factor, but the presence or lack of pessimism was deemed a possible, independent vital tool in stratifying CHD-induced mortality risk in the future.
The INTERHEART effort performed a large case control, 12,461 person, 52 country-wide study on the significance of anger, vigorous physical exertion and emotional upset in the hour before symptom onset of a heart attack.
-
It claims a population-attributable risk of 7.7% with strenuous physical activity and 8.5% with anger and emotional upset.
-
“Physical exertion and anger or emotional upset are triggers associated with the first” heart attack “in all regions of the world, in men and women, and in all age groups, with no significant effect modifiers.” It further asserts the consequence is additive if both factors are present during that critical time. (See reference study here).
Additionally, the “American Heart Association has stated that depression is an independent risk factor for a poor prognosis following an acute coronary syndrome.” A Harvard Health Publication extensively discusses the literary canon on optimism’s effect which proves a worthwhile read.
Key Points...
Not being a pessimist won’t guarantee being spared CHD (e.g. not smoking, preventing and controlling diabetes, maintaining optimal weight, keeping cholesterol levels and blood pressure down all help reduce your chances), but the perpetual high stress state it internally creates will certainly take an undesirable toll.
Focusing whenever possible on ways to improve your outlook – by finding strength in the lessons of your experience and personal fortitude, and control what is within your grasp can best serve you in many meaningful ways. By preserving your autonomy, you will maintain self-esteem and self-efficacy.
No one says this is always easy to achieve, but the practice and energy put toward the effort can be helpful.
For instance, getting an accurate diagnosis with correct staging and putting a treatment plan in place swiftly can mitigate much fear and the likelihood of PTSD. Or, expeditiously changing your doctor when you realize the relationship is not a fit. This should be a trusted rapport and without that it cannot be a therapeutic one. So, if a different doctor is what you need, then don’t fret or hesitate and make a switch. Having a supportive network of family and friends including your health care team is essential to your well-being. Doing activities that bring you joy on the days you feel up to it and surrounding yourself with positive influences are healing endeavors. Having no qualms about canceling a plan or saying no when it is a rough day are essential to self-care and optimizing your health. People will understand.
Being proactive, not reactive, in keeping your stress level down is a wonderful gift you can give yourself when enduring such trials. Fortify your mind and body with restorative measures (e.g. get proper sleep, eat nutrient-rich diet, exercise appropriate for your clinical state, be socially connected) and sprinkle laughter throughout your life, a remedy that cannot do you wrong! Writing your own story can flip the script, such is the power of resilience.
People will do and say things you don’t like, don’t take it personally. They are doing the best they can. Spend your time with those whose reactions are comforting to you. People cope differently.
Control What You Can Control
This can quell extra anxiety and worry. You can’t always change what is, but you can reduce the unnecessary concerns. And this is empowering. Ask for help. Don’t be afraid to say no. Give specific tasks. There will be good and bad days, prioritize your well-being. If someone has a negative impact on your mood, then control what scenario you put yourself in with that person. If someone energizes you and calms your fears, then spend more time with that person. If you don’t feel at ease broaching topics with your doctor, then change doctors and don’t agonize over the decision. Often bringing a third party to visits can be of great help in avoiding misinterpretation.
Go to this link for general guidance on how to talk to kids about your diagnosis.