By Ben Chan
Since bacteria, such as those that cause gonorrhea or gastrointestinal infections, are becoming increasingly resistant to antibiotics, scientists are searching for outside-the-box ideas to tackle the problem. They may have found in one in bacteriophage: viruses that exclusively infect and kill bacteria.
Bacteriophage (abbreviated “phage”) therapy isn’t new. It was originally used by Felix d’Herelle in the 1910’s to treat Shigella, a cause of dysentery. However, its clinical development all but stopped due to the discovery of antibiotics. The major reason is because antibiotics can kill a wide variety of bacteria, while phage are extremely specific. There were also issues with production, perceived inefficacy, and geopolitical concerns since phage therapy continued to be developed in what was then the Soviet Union.
But today, as our repertoire of effective antibiotics continues to dwindle, scientists are returning to their old friend, the bacteriophage. Are phage a potential solution to the global antibiotic resistance problem? Yes, quite possibly.
The single biggest benefit of phage therapy is that, unlike antibiotics which are just chemicals, phage are viruses. Though biologists disagree if viruses are technically “alive,” what is not doubted is that viruses can evolve. That means, in theory, if bacteria become resistant to phage, the phage will naturally evolve with the bacteria. How?
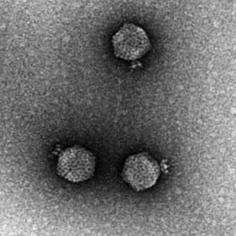
Bacteria and phage have been in an evolutionary arms race for billions of years. Phage cannot reproduce unless they have infected a bacterial cell. Many infections begin when a phage particle binds a bacterium and injects its own DNA into the cell, which essentially hijacks it. Under the command of enemy instructions, the bacterium turns into a virus-making factory, after which it explodes and dies.
Bacteria can become resistant to viruses in a variety of ways. One common mechanism is to alter the cell surface so that the phage can no longer bind. But the viruses are constantly changing, too. There’s a very good chance that if a mutant, phage-resistant bacterium evolves, a mutant virus that can still bind the bacterium also will evolve. In other words, as the bacteria try to evade the virus, the virus will keep trying new ways to infect the bacteria. Antibiotics cannot do this.
Another strategy to avoid the development of resistance is to use a phage “cocktail” – that is, a mixture of phage that each target a bacterium in different ways. (Similarly, we treat HIV infections by giving patients a “cocktail” of drugs that target the virus in various ways.) This strategy makes it difficult for bacteria to evolve resistance in the first place.
Another benefit of phage therapy is that prescribing the correct “dose” may not be much of an issue. With antibiotics, the correct dose is key. Too much, and the patient can suffer side effects; too little, and the bacteria survive and become antibiotic-resistant. But viruses can essentially dose themselves. If there are bacteria present, the viruses will infect them and multiply. If the bacteria are gone, the viruses soon will be gone from the body, too.
So why isn’t phage therapy conveniently available at any hospital or pharmacy? The short answer is that bacteriophage therapy isn’t approved by the FDA… yet. But clinical trials are now underway.
Phage exposure is believed to be safe. Just like bacteria, phage particles are absolutely everywhere. It is estimated that there are 1031 (ten million trillion trillion) phage particles on Earth, ten times more than the number of bacteria. The FDA, in fact, has given a product that consists of phage that kill Salmonella the “Generally Regarded as Safe” label.
It is easy to imagine that, in the not-too-distant future, we will greatly reduce our reliance on broad spectrum antibiotics and focus on personalized infection management. With the help of rapid DNA sequencing and Big Data, it may be possible to administer precision phage cocktails to treat bacterial infections.
Ben Chan is an Associate Research Scientist in the department of Ecology and Evolutionary Biology at Yale University.