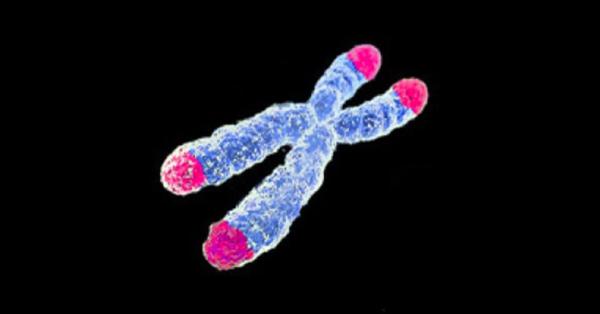
A new study in Translational Psychiatry sought to elucidate whether reduced telomere length (TL) is associated with childhood trauma in those with schizophrenia (SZ) and bipolar disorder (BD). Telomeres are the genetic material at the end of chromosomes that shorten in most human tissues with the wear and tear of aging. When they are excessively minimized, they don’t work as well and adversely impact a tissue’s ability to repair itself. Evidence shows a link between chronic stress and childhood trauma and accelerated TL shortening in otherwise healthy people (HC). This is why there is a ton of focus on studying it as a potential biomarker in the hope it can identify and ideally quantify “cumulative stress and biological aging.”
So, does this new research make a compelling case for its use in the real, not theoretical, world? Let’s just say the results, though intellectually interesting, wouldn’t necessarily change anything in clinical practice today.
What do we already know?
Chronic sustained high stress and extreme childhood trauma are known to do substantial harm. Persistently elevated levels of the stress hormone cortisol, for example, can weaken bones and muscles, increase risks of infection by impacting immunity, impair glucose metabolism, raise blood pressure, and alter mood and cognition. Untreated severe adverse childhood events can predispose a child to depression, anxiety, substance abuse disorders or other physical and mental health issues in adulthood.
The science supports the profound impact of toxic stress and childhood trauma in the later development of adult disease. It is widely known and accepted that the Adverse Childhood Experiences Study (ACE) “found a strong graded relationship between the breadth of exposure to abuse or household dysfunction during childhood and multiple risk factors for several of the leading causes of death in adults.” (See here).
From Best Practices to Breakthrough Impacts: A science-based approach to building a more promising future for young children and families by the Harvard University’s Center on the Developing Child is a compelling read. In it, the authors underscore how development is a highly interactive process where life outcomes are not exclusively set by genes. They extensively clarify the biological adverse effects which significant stress imposes on young children and families.
What did this new work reveal?
The authors conclude
“Our study confirms significantly shorter TL in a large sample of patients with SZ and BD compared with HC; however, the effect size is small. Shorter TL was specifically observed in patients reporting childhood abuse. No significant difference in TL was demonstrated between patients and HC after adjusting for childhood abuse. This suggests childhood abuse as an important factor for reduced TL in SZ and BD compared with HC...Patients reporting childhood abuse had the shortest TL, suggesting a link between early stressors and accelerated aging...We found no significant associations between TL and brain structures in our study”
It is unclear still what biological mechanisms contribute to this, though it is likely these early stressors cause intensified damage from oxidative stress due to escalations in cortisol levels or depletion of growth hormone (GH). But, there were many flaws in this study’s design, including but not limited to the following: TL was not determined from the brain but the circulating blood and drawing correlations has been shown to be inconclusive, confounders not adequately addressed, or methods for detailing childhood trauma were subject to recall bias.
Bottom line
The bottom line is childhood trauma, especially when untreated, poses a reverberating negative influence on physical and mental well-being well into an individual’s future. At this point, using TL as a biomarker in a clinical capacity in the realm of SZ or BD is premature and wouldn’t yield great or practical dividends.
Source: Monica Aas, et al. "Telomere length is associated with childhood trauma in patients with severe mental disorders." Translational Psychiatry 9, Article number: 97. Published: 21-March-2019. DOI: 10.1038/s41398-019-0432-7