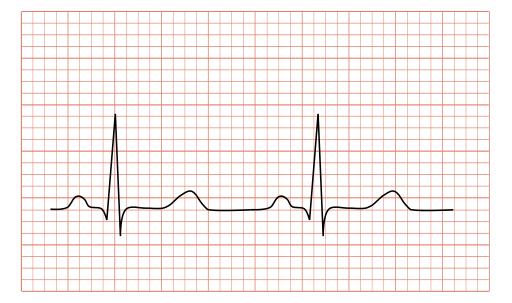
Electrocardiograms, ECGs, are one means of capturing information about the function and structure of the heart by looking at the heart’s electrical activity. But can it, like the chest x-rays I wrote about previously, contain hidden information? A new study in Circulation argues that it can.
It is an artificial intelligence study, so you know the drill, roughly 500,000 12-lead ECGs used for training and validation; 275,000 used for testing. Mean age of participants, 58.6, slightly more males. It is also a bit of a fishing expedition, searching for “novel uses of the ECG” – harnessing factors that alter the electrical conduction and therefore the ECG, like a patient’s potassium level or enlargement of the heart itself. The question asked, could the ECG alone predict the patient’s age and gender?
- Algorithmic evaluation of the ECG could accurately predict a patient’s gender 90% of the time. Of course, reading patient identification would increase that accuracy to 100%. The clinical value of algorithmic identification of gender is unclear. But it adds to our understanding that women are physiologically different from men, in unsuspected and under-investigated ways.
- The AI evaluation of age was around 94% give or take about seven years. Again, reading the patient identifier or even asking the patient would increase the accuracy to 100%. But here the researchers were able to turn lemons into a “sort of” lemonade.
They took a more in-depth, exploratory dive into 100 patients who had serial ECGs over 20 years. They looked into their medical records matching ECGs to their changing health. For this group, they found that for those where the ECG predicted age was closer than seven years, there were very few, if any comorbidities. In the year, that there was an untoward event, like new-onset hypertension, diabetes, or a heart attack the error in predicted age rose, then once the patient “stabilized,” the predicted age returned to its previously erroneous baseline. Patients with an age error greater than seven years had a statistically significant higher incidence of comorbidities.
All of these findings, easily found in a patient’s history, suggest that medical problems can become additive and reflected in subtle ways we do not anticipate. While noting that physiologic age is different than chronologic age, the researchers stretch that connection suggesting that the ECG age predictor reflects those differences. Not a bad recovery from data that was only 90% accurate for its intended purpose, calculating age.
Like other AI breakthroughs, the how and why of the algorithm remains a black box, “a complex set of factors that include varying levels of non-linear interaction.” Both this study and the chest x-ray study I mentioned previously fit within a more extensive belief system. As we age, there are subtle, non-clinical alterations in our physiology that accumulate over time into phenotypic changes, going bald, abnormal clotting, elevated cholesterol, your weight, the possibilities are endless. Studies have shown that a simple accounting of those type of chronic changes, irrespective of whether they are seemingly trivial, like baldness, or touted as significant risk factors, like cholesterol or a stroke, can quantify physiologic aging. AI may bring some mathematical subtlety to the quantification, changing a linear additive aggregate into some interactive non-linear equation but it does not give us a direction in which to move, it remains more odometer than a map. Now that AI has increasingly demonstrated its basic capabilities; its value will be found in how it guides us, not in how it magically identifies where we are.
Source: Age and gender estimation using artificial intelligence from Standard 12 lead ECGs Circulation DOI: 10.1161/CIRCEP.119.007284