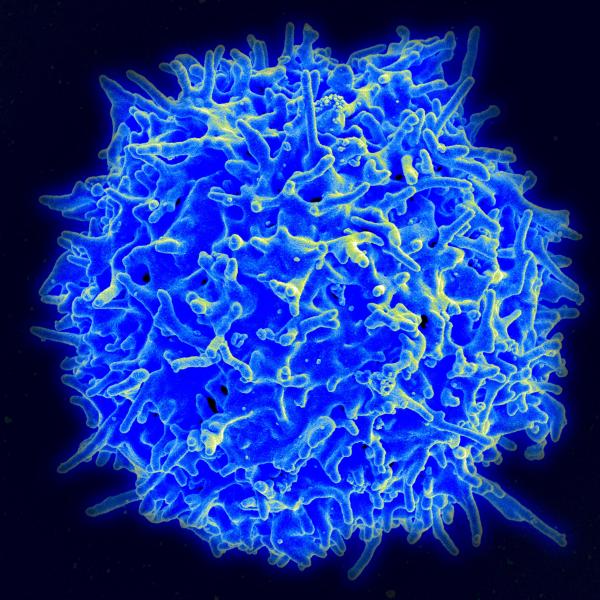
We rarely take a moment to reflect on the beauty, indeed, the awe-inspiring nature of what makes us tick. And while all of our physiologic systems are intricate shorelines that we can continually discover and reimagine, our immune system is perhaps the most elaborate. Immunity stands at the portal where our inner selves meet and interact with all of the outside worlds, all of the other. While one group of scientists have attempted to understand immunity through its finest detailing, bringing us vaccines, antimicrobials and now CAR-T therapies; other scientists continue to search for the evolutionary underpinnings of immunity. By the mere facts that we breathe and eat, we are integrated into our environment; immunity helps to regulate that integration.
There are two competing theories in understanding our immune system at a high level. There is the barrier hypothesis, where the skin, lungs, and gastrointestinal tract serve as borders separating our internal “us” from outside “other.” When those defensive perimeters are breached, the immune system, like Paul Revere and the Minutemen, a cellular army comes out in force in our defense. One is viewing it as a barrier, and another is seeing it perhaps as more a sensory organ. The military analogies are not accidental, as immunology came of age between World War I and the cold war when those analogies were particularly apt. Our cultural metaphors played a significant role not in identifying the particular facts of the immune system’s workings, but in crafting the narrative, the hypothesis which sought to tie the dots into a picture.
Allergic responses are easily understood as “barrier” diseases. Think of how your skin reacts when it is exposed to poison ivy, or how sensitive individuals will respond to gluten or peanuts. Sepsis, among its many alterations of our self, loosen the connections between the cells of the intestinal tract, the breakdown in the barrier allowing many more bacteria to reach our bloodstream.
The second theory, the hygiene hypothesis, developed as our understanding of ecologic systems became ascendant, requiring new metaphors, and prompting new observations. The barrier theory is more like Cortez’s invasion and conquering of the Mayans; the hygiene hypothesis is more my generations first trip to Europe, backpack, hostel, sampling food, and culture to broaden our horizons. The barrier theory says that food fallen onto the floor is  disgusting; the hygiene theory states that the food is edible if you pick it up quick, especially if it is tasty.
disgusting; the hygiene theory states that the food is edible if you pick it up quick, especially if it is tasty.
Immunity’s primary function shifted from defense to vigilance in a changing world. Our immune system senses our environment in the same way our ears sample sounds, and our eyes sample light. Building upon that metaphor, immunity is a perception, and as we have learned from optical illusions, our sensory systems can be fooled into seeing things that are not there. The hygiene hypothesis’ immune system is more mediator than a soldier or at least rebalances the role those two functions serve.
Both are theories; neither is complete or proven; their most significant value is in introducing us to new ways to view our immune system.
Why are peanut allergies increasing?
Peanuts are native to South America and spread to Europe and Africa by the Spanish, but there is evidence of our having eaten them for 7600 years. While that period seems long on a cultural time-scale; on a genetic time-scale, it is a fractional moment. So, it is hard to see how we can ascribe increasing peanut allergies solely to genetics. Some have attributed the rise of peanut allergies to the fact that infants are not exposed to these proteins earlier enough. Is it possible that a mismatch between our older genes and our newer environment can be an underlying source of this problem? Over that same period, there have been two global cultural changes.
First, we have sanitized our food sources and overall hygiene. Leave processing and additives aside; we simply are less exposed to microbes and parasites. And in the same way that agriculture has allowed us the free time to develop water treatment, sewage systems, and a host of antimicrobials, it has freed of from being obligate predators – we no longer have to walk around all day to stay alive, or work in a field to bring in a harvest.
There is increasing evidence that dietary changes alter our gut microbiome, a source of hormonal regulation with the nervous system, a sensory organ for the ingestion of our environment. Hygiene has altered the flora that lives within us. While scientists refer to this as a biome depletion, depletion is a relative term, but it certainly is a change. The hygiene hypothesis suggests that those alterations have in turn, altered our immune system and how it recognizes us from them.
There is abundant evidence that we are less active; there were no spin classes or fitness trainers 100 years ago. The hygiene hypothesis is asking if it is not the mismatch of those changes in our diet and exercise, with our ancient genes that give rise to some of our current maladies, those Western diseases, obesity, diabetes, and autoimmune diseases. Can it be that the great medical homilies are the ground truth, that our health depends on our diet and using our body?
We are holobionts – assemblies of various organisms
Our energy factories, the mitochondria, have distinctly differently genetics from the human genome, and indeed the bacteria that inhabit our GI tract are among the many “creatures” that form the cooperative we call us, and scientists call holobionts. It is not difficult, knowing this, to recognize that our evolution is intimately tied to their evolution, we have co-evolved. It is reasonable to suggest that our genetic heritage is based on what other species we encountered and how we viewed them. One need look no further than the Black plague or the 1918 Influenza epidemic to see how pathogens can drastically alter human conditions.
The hygiene hypothesis suggests that our immune system works best when it has been exposed to a diversity of foreign others; and that population measures of hygiene, such as running water, waste disposal systems have not so much weakened as altered our responses. More specifically scientists ask whether today’s environment causes “biome depletion” – a loss in the diversity of others. And that brings us to a rarely considered, “tropical disease,” which affects roughly 30% of the world’s human population, helminth parasites, worms.
Now, these hidden travelers often join humans early in life and result in chronic infections. The fact that they are “on board” before our reproductive years means that they can influence our genetic makeup; after all, if you are very susceptible to them, you just do not have the opportunity to share your genes with the next generation. Helminths have been shown to both upregulate and downregulate our immune response so it is a tantalizing idea that an absence of worms may cause our immune system to become out of sync. More specifically, there is evidence that helminths down-regulate the immune system and reduce the incidence of autoimmune diseases and allergies, both of which are more frequently seen in developed, “Westernized,” societies.
I hasten to point out that the current status of “the science,” in this area is contradictory and muddled. In some instances, worms act to upregulate and in others to down-regulate. The situation is further confounded by the fact that helminths are a diverse group and experimentation has involved not only a range of these creatures but several animal models as hosts. One of the hurdles, as you would expect, is finding human hosts for study. That has led to attempts to isolate the various metabolites spawned from helminths to detect a chemical that we might synthesize and use as an immune modulator.
Helminth therapy is not yet ready for prime time, even though several clinical trials have been initiated. But it does give one a moment to pause. There is much more to learn about the intricacies of our immune system and how it is shaped and shapes our environment.
Next up, a modern twist on the idea that women are prone to their own set of diseases. Are autoimmune diseases a variation on hysteria?