For those of you, a bit late to the party, I recently wrote on the push by the AMA and the Association of American Medical Colleges to guide the formal speech of healthcare workers. This most recent study examines the most ubiquitous words of our written speech, the short narrative that is our admission notes for a hospitalized patient. These notes summarize the circumstances leading to the patient’s admission and serve as a means of communication between clinicians.
The researchers in the current study used natural language algorithms to search for stigmatizing language in all inpatient admission notes of an academic medical center and three subgroups: patients with diabetes, a substance use disorder, or those being treated for chronic pain. The lists of stigmatizing words come from guidelines developed by the American Diabetes Association, the Association of Diabetes Care and Education Specialists, and the National Institute on Drug Abuse [1]
The Findings
- THE dataset included 48,651 unique admission notes on 29,783 individual patients (1.6 admission notes per patient), written by 1932 clinicians (a median, nine admitting notes each). Physicians, who ranged in training from medical student to attending with a mean of 5 years since graduation, wrote 87.4% of those notes.
- Stigmatizing Language was found in 2.5% of all notes: 6.9% of notes for patients with diabetes, 3.4% in patients with a substance use disorder, and 0.7% in patients with chronic pain.
- Non-Hispanic Blacks' records had a greater probability of having stigmatizing words than non-Hispanic Whites. The absolute increase was 0.67%, but the relative increase was 26.8% - you chose the number you wish to consider.
- For every 1-point increase in the severity of diabetes (a measure of how easily diabetes can be managed), there was a 1.23% increase in stigmatizing language. The increase was 2.11% for non-Hispanic Blacks with diabetes compared to non-Hispanic Whites with diabetes.
- For patients with a substance use disorder, non-Hispanic Blacks had a 2.16% increase in stigmatizing language over their non-Hispanic White cohort. For those in chronic pain, the disparity was 1%.
Of course, we have not even considered the stigmatizing words themselves until now. The researchers offered their table of terms, but it is unenlightening because it was alphabetical. I have reduced the list of 60 words to those responsible for 80% of the stigmatizing usages. As you will see, the same note often contained the same word many times.
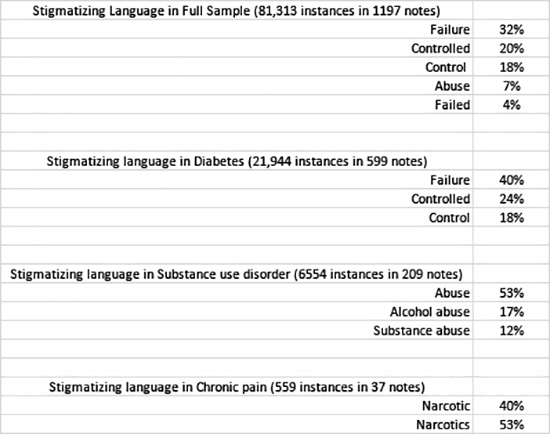 In admissions for diabetes, the stigmatizing words reflected the state of diabetes management without further context. The researchers didn’t examine whether the language explicitly “blamed” the patient for those failures. For example, the "failure" of management and a loss of blood sugar control can be due to the prescribed treatment regimen, just as it might be due to a patient’s noncompliance (another stigmatizing word) with my recommendations. For admissions for substance use disorder, the keyword is abuse which is no longer used in medical diagnosis after it was felt to be too pejorative by the American Psychiatric Association. For admissions for pain, narcotic is the trigger word. But according to the CDC:
In admissions for diabetes, the stigmatizing words reflected the state of diabetes management without further context. The researchers didn’t examine whether the language explicitly “blamed” the patient for those failures. For example, the "failure" of management and a loss of blood sugar control can be due to the prescribed treatment regimen, just as it might be due to a patient’s noncompliance (another stigmatizing word) with my recommendations. For admissions for substance use disorder, the keyword is abuse which is no longer used in medical diagnosis after it was felt to be too pejorative by the American Psychiatric Association. For admissions for pain, narcotic is the trigger word. But according to the CDC:
“Narcotic drugs – Originally referred to any substance that dulled the senses and relieved pain. Some people use the term to refer to all illegal drugs but technically, it refers only to opioids. Opioid is now the preferred term to avoid confusion.”
The researchers offered alternative words. Opioids can be used in place of narcotics, although to me, that is a distinction without a difference. Abuse can be replaced by misuse; maybe that is perhaps somehow softer and less stigmatizing, if at all. There were no suggestions to replace the three biggest offenders: failure, controlled, and control.
Here is an interesting paradox. In the guidelines written by the AMA and AAMC, some terms were deemed too dispassionate and required an attached value judgment. As the authors of the guidelines wrote about health inequities:
“health differences that are unjust, avoidable, unnecessary, and unfair—no longer a simple calculus of difference, but an assessment based on a value judgment.” [emphasis added]
But for the current researchers, all of these stigmatizing words contain value judgments, which is the essence of using the word stigmatizing. In some instances, we need to inject our values; in others, we should not – I suppose it comes down to which values we are injecting.
We should also consider the suggestion by the researchers that there is a bias among clinicians and that we are more stigmatizing to non-Hispanic Blacks than non-Hispanic Whites. Here is the figure from the paper:

Remember that if the horizontal line reflecting the range of values touches the vertical axis with this form of plot, it has no significant meaning, statistically or clinically. The right column shows the breakdown by those three disease subgroups. Only the term "refused" as compared to refuses demonstrates a disparity in usage between those non-Hispanic Blacks and Whites in patients with diabetes. No word shows a significant difference for those patients with chronic pain or a substance use disorder.
Consider the words of the researchers when discussing the limitations of the study:
“Our dictionary-based natural language processing approach allowed us to identify the frequencies and patterns of stigmatizing language use, but some instances of stigmatizing Language we captured would not be viewed as stigmatizing in context. Moreover, it may be challenging for physicians to accurately document patients’ care without the use of stigmatizing words, such as nonadherence, and many things that should be documented in patients' records (e.g., substance use disorders) might be somewhat stigmatizing even if written in the most respectful way possible.”
In the absence of context, we don’t know whether these words were stigmatizing at all. It would be best if you did more than run a computer algorithm across a dataset to get at the context. You need to actually read the “flagged” note and make a judgment call. There are ways of minimizing bias in those judgments, even if they are flawed. Those results would be of value. At least to me, these results are more “the sound and the fury.” It serves to pad a CV and provide clickbait but offers no substantial understanding or insight.
[1] It is somewhat ironic that the National Institute on Drug Abuse has a stigmatizing word, abuse, in its name – perhaps a do as I say, not as I do moment.
Source: Examination of Stigmatizing Language in the Electronic Health Record JAMA Network Open DOI: 10.1001/jamanetworkopen.2021.44967




