Before jumping into Dr. Bastard’s research, we need a few background definitions.
Interferons are the Paul Reveres of our immune defenses. Interferons are signaling proteins that belong to the larger family we call cytokines – the cell’s communication network. They were named because of their ability to interfere with viral replication by signaling to the surrounding cells to increase their anti-viral defenses. Not to be easily defeated, some viruses can blunt interferons activity to facilitate greater “infectability.”
Interferons can be further categorized, but it is sufficient to mention Interferon Type 1; produced in response to immune recognition of a virus and prevent “the virus from producing and replicating its RNA and DNA,” and help regulate and activate our immune defenses. Those functions follow a specific time-course as the interferons first cause local protection of cells and later downstream defenses in other areas. COVID-19 provokes a more muted response by interferons than other viruses, which may help explain, in part, its infectability. More interestingly, a delay in interferon’s response “contributes to the pathogenic inflammation” we call cytokine storm.
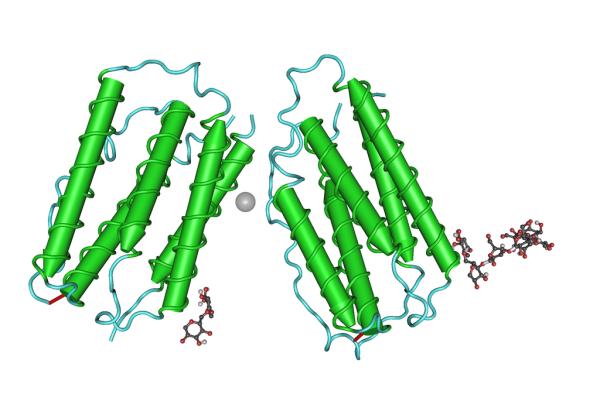
Another cytokine family member are interleukins; there are currently 17, all derive from white blood cells, hence leukin; all act as communicators between cells, hence inter. Interleukin 6 is a protein and sugar, a glycoprotein, that, among other functions, is involved in helping B cells differentiate to make antibodies against foreign invaders, like viruses. Interferon 7 promotes both B cells and our immune memory cells, the T cells, and can play an important role in getting out “the troops” in our adaptive immune responses.
The COVID Human Genetic Effort (CHGE) is a collaborative study of our exome, a subset of our genome, where 85% or so of the mutations thought to cause disease reside. It looked at patients with either mild or severe clinical manifestations of COVID-19, searching for inborn errors of immunity. Among those individuals with life-threatening COVID-19 infections, they found alterations in the effectiveness of interferons overall and an X-linked variant, therefore found only in men, that resulted in deficient Type 1 interferon production. Three additional studies bolstered their work
- In a study of 987 individuals with life-threatening COVID-19 infections, 10% had auto-antibodies to Type 1 interferons – autoantibodies preventing interferons from stopping COVID-19 in vitro.
- A study of patients with autoimmune polyglandular syndrome type-1 (APS-1) which produces auto-antibodies against Type 1 interferons. Of the 22 patients aged 8 to 42, 86% were hospitalized, 68% were placed in intensive care units, 50% were on ventilators, and 18% died.
- A study of 34,000 uninfected individuals found that auto-antibodies to Type 1 interferons increase with age. It rose from 0.18% in those 18-69 to 3.4% in those over 80. When adjusted to the ability to neutralize physiologic amounts of interferon, that 3.4% rose further to 6.4%.
Dr. Bastard suggests that if we could (we can, it is a matter of will) identify these individuals, we could target our protection, and perhaps therapy, more strategically. For us, the importance of these studies is that disease susceptibility, in this case, COVID-19, is multi-factorial involving genetics, our environment, and lifestyle choices. There is rarely the causative factor; there is always a multiplicity. Moreover, slight variations can have significant downstream impacts. We should be more humble and less strident about what we do and do not know. Humility in the face of our known and unknown biology should get the partisans to speak more equably and with less certainty; it won’t, but it should.
Source: Why do people die from COVID-19? Science DOI: 10.1126/science.abn9649