If your family or friends have not been touched by Parkinson’s Disease, a neurologic disorder characterized by uncontrolled or unintended movement, Michael J. Fox is the person that might come to mind. This is particularly salient here because it was the Michael J. Fox Foundation for Parkinson's Research that was the primary mover and funding partner of this work. Before describing the new findings, a quick Parkinson’s primer.
Parkinson’s Disease
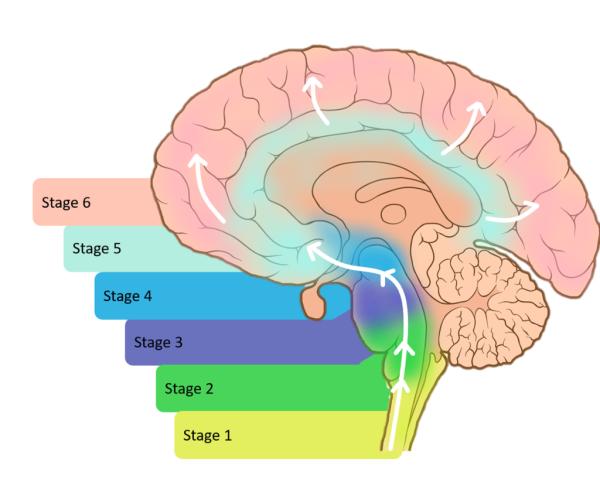
The underlying cause of those uncontrolled or unintended movements is when brain cells stop producing dopamine, resulting in a variety of symptoms. While not an orphan disease – it impacts roughly one million in the U.S. – it is overshadowed by many other life-altering conditions. We do not know why this loss of function occurs, but it is a tangle of genetics, environmental factors, and aging, its most significant risk factor. Among the "malfunctioning" genes associated with Parkinson’s is the alpha-synuclein gene (SNCA). Alpha-synuclein accumulates in the brain of nearly all patients with Parkinson’s. This is the biomarker that is the subject of the study. [1]
Parkinson’s Disease is a clinical diagnosis; there is no finding in the blood, cerebral spinal fluid (CSF), or imaging technique that confirms the condition. The Parkinson’s Progression Markers Initiative (PPMI) was founded to seek biomarkers that could help in the search to understand and treat Parkinson’s and include 1,400 patients who have undergone a range of biosampling and imaging. They are the cohort reported. PPMI is an example of collaboration between patients and pharmaceutical companies.
While the hallmarks of Parkinson’s are the motor dysfunctions of stiffness, resting tremors, and slowness, other “invisible” symptoms of PD can affect our autonomic nervous system. It can impact mood, memory, thinking, your ability to eat and sleep, and a decreased ability to detect odors – hyposmia. With a plethora of symptoms, the presentation and course of Parkinson’s are unique to each patient.
“Recognizing heterogeneity in underlying pathology among patients with Parkinson’s disease has been a major challenge. Identifying an effective biomarker for Parkinson’s disease pathology could have profound implications for the way we treat the condition, potentially making it possible to diagnose people earlier, identify the best treatments for different subsets of patients, and speed up clinical trials.”
- Andrew Siderowf, MD, Chief Movement Disorders Division of Neurology Perelman School of Medicine
The 1,123 participants in the study included:
- 545 patients with Parkinson’s Disease, including those without genetic links (sporadic cases) and those with genetic linkages to GBA and LRRK2
- 54 with Parkinson’s Disease without evidence of Dopamine Deficiency on brain scans
- 51 without Parkinson’s but with early signs, specifically loss of smell and sleep disorders – prodromal patients
- 310 without Parkinson’s but with known genetic variants – non-manifesting carriers (NMC)
- 163 healthy controls
The accumulation of misfolded alpha-synuclein (termed αSyn seeds) is a pathologic hallmark of Parkinson’s found in the brain, most often at autopsy, as the brain is infrequently biopsied. The biomarker is the misfolding detected in the CSF, based on an amplification technique used to identify another group of misfolding diseases, prion disease (think Mad Cow Disease), like Creutzfeldt-Jakob disease, a rapidly fatal neurodegenerative disease. The value of the biomarker had been established in earlier small studies demonstrating it could separate healthy controls from those with Parkinson’s disease; this is the largest cohort studied. This is the first biochemical test to accurately diagnose Parkinson’s among the living.
- The new test, αSyn-SAA, had a sensitivity (true positives) of 87.7% and a specificity (true negatives) of 96.3% in all patients diagnosed with Parkinson’s Disease.
- For sporadic Parkinson’s, those without a genetic linkage, 93% of individuals had a positive αSyn-SAA result
- For those with the GBA variant, there was a 96% positivity, 68% for those with LRRK2
- Most prodromal patients were αSyn-SAA positive, especially among those with hyposmia at 89% and sleep disorders at 85%. No similar association was found for other clinical findings, including alterations in autonomic function, cognition, and depression. Among non-manifesting carriers with variants but not symptoms, roughly 8% were αSyn-SAA positive. [2]
This test accurately identifies those with Parkinson’s Disease from healthy controls and can help more accurately stratify patients. It supports the idea that there is a long prodromal period before the development of clinical signs and symptoms that might allow for intervention to mitigate the disease.
“Taken together, these findings have immediate implications for clinical trial design, both to identify pathologically defined subgroups of PD patients and to establish biomarker-defined at-risk cohorts. Longitudinal research is needed to investigate the prognostic value of αSyn- SAA and whether changes in quantitative measures of αSyn aggregation indicate progressive pathology over time.”
[1] Other genetic variants include PRKN, found in younger Parkinson’s patients, and GBA and LRRK2, found in Eastern European Jews and North Africans of Berber descent
[2] One of the earliest biomarkers of Parkinson’s is a brain scan showing diminished dopamine-producing nerve cells, but given these findings, it may well be that α-synuclein aggregates are an even earlier diagnostic finding.
Source: Assessment of heterogeneity and disease onset in the Parkinson’s Progression Markers Initiative (PPMI) cohort using the α-synuclein seed amplification assay: a cross-sectional study Lancet Neurology DOI: 10.1016/S1474-4422(23)00109-6