Traffic-related air pollution (TRAP) refers to pollutants from vehicle sources like exhaust and brake/tire wear, including ultrafine particles, black carbon, nitrogen oxides, carbon monoxide, carbon dioxide, and, to a lesser extent, the badboy pollutant, particulate matter, specifically PM2.5. TRAP is the most common source of urban air pollution, and because of uneven dispersion, it clusters around roads and highways. [1] TRAP exposure is acknowledged as a cardiovascular disease risk factor, potentially mediated through inflammation and alterations of our neural responses (autonomic dysregulation). Given the average travel time to work is 27 minutes, many get a dose of TRAP twice a day.
 To consider the impact of TRAP on our blood pressure, researchers drove participants on a defined route through Seattle for 2 hours, beginning at 9:30 AM. Their car was closed to outside air, and all air entering it went through one of two possible filtration systems. The first was simply air through the car’s ventilation system with all filters removed. The second was the same setup, but now there were two filters: a conventional car filtration system and a HEPA filter capable of removing particulate matter and carbon. Participants and their drivers were blinded as to the presence or absence of the filters, and each participant was driven around on three occasions, twice without a filter and once with the filtration system. It was, therefore, a double-blind crossover study.
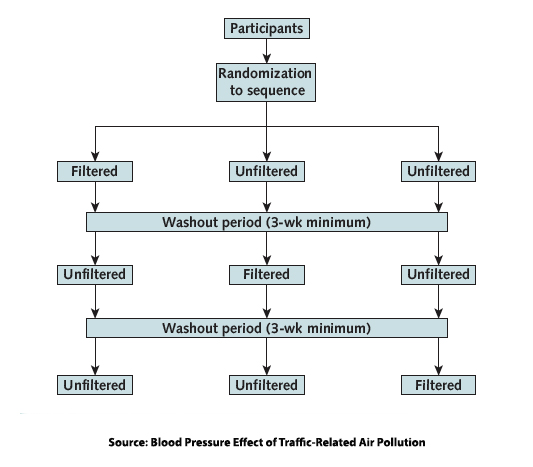
To consider the impact of TRAP on our blood pressure, researchers drove participants on a defined route through Seattle for 2 hours, beginning at 9:30 AM. Their car was closed to outside air, and all air entering it went through one of two possible filtration systems. The first was simply air through the car’s ventilation system with all filters removed. The second was the same setup, but now there were two filters: a conventional car filtration system and a HEPA filter capable of removing particulate matter and carbon. Participants and their drivers were blinded as to the presence or absence of the filters, and each participant was driven around on three occasions, twice without a filter and once with the filtration system. It was, therefore, a double-blind crossover study.
One strength of the study was that it was conducted in the real world, not a laboratory. On the other hand, there were only 16 participants, aged 18 to 49 years, reducing the “power” of the research conclusions. While the researchers considered several physiological measures, the report limits its discussion to blood pressure primarily because it was the most clinically relevant outcome. Blood pressure was taken using a device that measures pulse waveform, like a pulse oximeter, rather than a cuff, allowing consistent measurements while driving. [2] Measurements were made before, during, and after being driven in traffic – 14 measures over 24 hours.
Participants had a mean age of 29.7, and there were essentially equal numbers of men and women. The means systolic BP was 122.7 mm Hg, diastolic 70.8 mm Hg. There were “modest imbalances by age and blood pressure” concerning the specific drive sequences, i.e., when the unfiltered drive occurred in the sequence of three rides. The filtration systems were particularly effective in removing particles; overall, particles were reduced by 86%, black carbon (soot) by 86%, and PM2.5 by 60%. Filtration had a minimal impact on NO2, a 19% reduction, and no impact at all on CO or CO2.
Results
- Raw mean blood pressure values generally decreased in both groups; there were larger decreases in the filtered group.
- The peak effect was experienced 1 hour after the start of the drive for systolic and diastolic blood pressure.
- Systolic and diastolic blood pressure was generally 4.5 mmHg greater on unfiltered drives.
- After 24 hours, there remained a persistent elevation of blood pressure in the unfiltered drive group, more for the diastolic than systolic blood pressure.
Some takeaway thoughts
The researchers looked back at their prior study of the impact of diesel fuels on blood pressure and felt that ultrafine particles rather than PM2.5 might be the drivers of hypertension. The EPA does not explicitly regulate these particles; they are subsumed in PM2.5.
The raw data presented showed that the baseline blood pressure prior to the drive in either a filtered or unfiltered car was elevated. All the blood pressure measures while driving were lower. (Could this mean driving in traffic reduces blood pressure?)
I wrote to the authors, who indicated that these elevated results were calculated based on comparing an individual’s blood pressure response in an unfiltered vs. a filtered environment at the same point in time and presumably at the same point in the drive. To my mind, this muddies their conclusion:
“…unfiltered exposure may result in net increases in blood pressure…”
because these increases were relative to one another; overall, blood pressure was lower while driving. [3] I asked the authors about this, and they responded:
“When anybody is sitting at rest, as when they are passengers in cars, their blood pressure generally goes down from the time they get into the car to when their body systems re-equilibrate to the new position.”
A valid point, but then why were the measurements not made after the individual had entered the vehicle but before the drive began? It is a small study, and despite the reporting in the mainstream media, it did not involve ‘rush-hour” traffic. Most importantly, from a clinical perspective, as the authors acknowledge,
“The clinical implications of transient changes in blood pressure are not well understood.”
As with all good science, the study raises more questions than providing answers. It does involve real-world conditions, but whether a transient difference in blood pressure has long-term clinical implications remains conjecture.
[1] That is why one “social determinant” of our health, proximity to highways, is a concern.
[2] You can find out more about pulse waveform blood pressure readings here.
[3] Reminiscent of Washington speak where an increase in funding that is not as great as desired is a decrease.
Source: Blood Pressure Effect of Traffic-Related Air Pollution Annals of Internal Medicine DOI: 10.7326/M23-1309




