“We have very clear evidence that, though not risk free, nicotine e-cigarettes are substantially less harmful than smoking.”
- Hartmann-Boyce Ph.D. Lead Author and Assistant Professor of Health Policy and Management University of Massachusetts Amherst
Perfection is the Enemy of Good
In a perfect world, no one would smoke tobacco, which has enormous costs to individuals, their families, and public health funding. But our world is far from perfect, and any means to reduce harm by helping smokers quit should be considered. Vaping, the verb for electronic cigarette’s noun, is often portrayed in a bad light when conflated with the vaping of substances other than tobacco that have more sketchy manufacturing pedigrees. ACSH feels that on balance, given the benefits as well as the currently known adverse effects, vaping nicotine contributes to harm reduction because it aids in the cessation of smoking tobacco.
What is Cochrane Reporting?
The study is limited to e-cigarettes (ECs), devices “producing for inhalation an aerosol formed by heating an e‐liquid using a battery‐powered heating coil.” More specifically, they contain nicotine, glycerol or propylene glycol, and sometimes flavors. More importantly, for efforts at cessation, ECs look and feel like cigarettes, and they can often be used in the same settings as the use of tobacco – with that morning cup of coffee, taking a break with co-workers, after dinner, etc.
It is part of a continuing analysis of the harms and benefits of ECs begun by Cochrane in 2016 and meant to enter the scientific discourse around ECs, where some, like the US Preventive Services Taskforce, concluded
"that the current evidence is insufficient to assess the balance of benefits and harms of electronic cigarettes (e‐cigarettes) for tobacco cessation in adults"
- (USPFTS 2021).”
The meta-analysis involved 78 studies, 17 new since Cochrane’s prior update, and 61 studies reviewed previously or with updated information. Overall, more than 22,000 adult participants, predominantly in the US; 22 randomized controlled studies, 7 cross-over designs, and the rest observational studies. 72% of the identified funding is from non-industry sources. As is inevitable, there were varying degrees of bias. Here is the Cochrane summary on bias.
 And they neatly tied together the results in a graphic:
And they neatly tied together the results in a graphic:
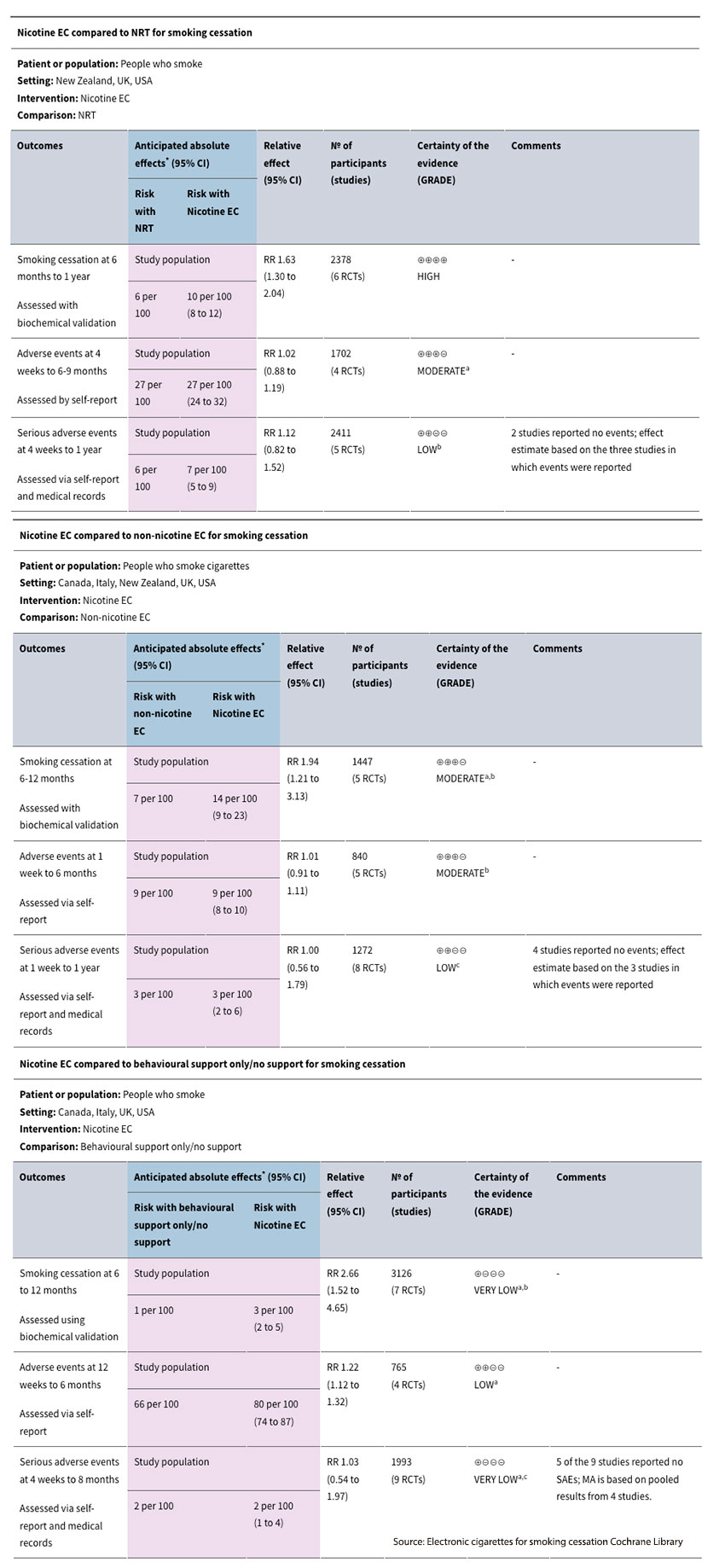
Focusing on the column labeled "Relative Effect", the use of ECs containing nicotine was better at reducing smoking cessation six months after intervention than both nicotine replacement therapy (NRT), e.g., nicotine-containing gum, and the use of ECs without nicotine. It was also far better than simple behavioral support, but the evidentiary quality was low – conclude as you wish. Stated in more practical numerical terms
“…an additional two to six people for every 100 would quit smoking with nicotine EC compared to NRT, an additional two to sixteen people for every 100 would quit smoking with nicotine EC compared to non‐nicotine EC, and an additional one to four people for every 100 would quit smoking with nicotine EC compared to behavioural support only or no support for smoking cessation.”
What about harm?
The Cochrane researchers reported that the use of nicotine-containing ECs was not associated with an increase in adverse or seriously adverse consequences compared to NRT or non-nicotine ECs. However, and this is critical, there was a lack of data, making conclusions of low certainty. More importantly, there is also a paucity of long-term data. A companion meta-analysis referenced by Cochrane looked at various biomarkers, e.g., carbon monoxide, nitrosamines, and other metabolites of polyaromatic hydrocarbons – you know, the bad stuff concluded:
“Switching from smoking to vaping or dual-use appears to reduce levels of biomarkers of potential harm significantly.”
Inhaling the combustion products of tobacco is stupid; it is also addictive. The use of aerosolized nicotine from vaping makes it easier to end an addiction. The adverse consequences of vaping remain uncertain, but the absence of evidence is not evidence of absence. More studies need to be done. The current thinking from Cochrane’s analysis is that vaping, even dual use with tobacco, reduces the unhealthy biomarkers associated with smoking tobacco. Tobacco smoking remains the most significant preventable cause of death in the US. The FDA has approved several medications to aid in smoking cessation; e-cigarettes have not been given such approval. In the personalized treatment of tobacco addiction, which remains a real menace, vaping nicotine remains a useful tool.
Source: Electronic cigarettes for smoking cessation Cochrane Library




