Modern medicine has produced many kinds of high-tech miracles, among them gene therapy to correct malfunctioning genes, electrical stimulation devices to restore significant function after traumatic spinal cord injury, surgery performed using robots, and a wearable, postage-stamp-size ultrasound patch that can take real-time images of the heart and monitor its performance.
Another sector of medicine that desperately needs breakthroughs is the transplantation of solid organs, which are in severely short supply. Currently, more than 100,000 Americans are waiting for transplants, and due to a shortage of hearts, lungs, livers, and kidneys, at least 17 die each day. Donor organs — from a living person or cadaver — must match the rejection recipient’s tissue type and size; they are often not perfect. By one estimate, approximately half of transplanted organs are rejected by recipients’ bodies within 10-12 years, despite a constantly expanding understanding of what causes rejection. Another obstacle is that the organ procurement system in the U.S. is inefficient, inconsistent, and unaccountable – in short, a mess that causes preventable deaths.
We are making progress, but too slowly. Two new high-tech approaches to providing organs for transplantation might ultimately both eliminate the need for organ donors and reduce the risk of tissue rejection. And there is also a low-tech approach that would require only a tweak in healthcare policy.
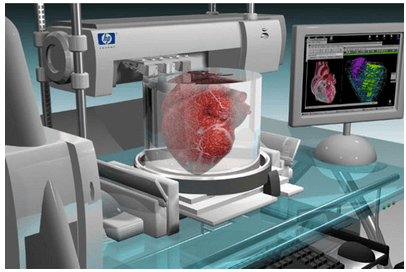
Organs produced by 3D bioprinting
The first of the high-tech approaches is three-dimensional (3D) bioprinting, which uses “bio-ink,” a printable material made from a patient’s own cells, to print layer upon layer, creating tissue the recipient will not reject. But in progressing from tissue to a complex organ, one critical challenge has been creating blood flow to keep the cells alive; researchers have devised several approaches, which include threading tiny channels through the organ, where blood vessels develop when implanted in animals, or seeding channels with the endothelial cells lining the inside blood vessels.
An exciting advance was reported by a Swedish research group attempting to create human lungs by 3D printing. According to the lead author of the study,
We started small by fabricating small tubes, because this is a feature found in both airways and in the vasculature of the lung. By using our new bioink with stem cells isolated from patient airways, we were able to bioprint small airways which had multiple layers of cells and remained open over time.
The fabrication of other organs presents additional, more imposing obstacles. The liver and kidneys produce hormone-like substances that modulate physiological processes such as blood coagulation, blood pressure, and removing toxins from the bloodstream. It is difficult to see how these closely regulated functions could be incorporated into 3D-printed organs.
Credit: Centromere121 via CC-BY-SA-3.0
In addition to the daunting technical challenges, healthcare executive Daniel Troy has described the regulatory lassitude at the FDA as one that has discouraged commercial interest in the field. He observed that while the FDA is accustomed to evaluating the safety and efficacy of mass-produced therapies and medical devices, “bioprinted organs are one-of-a-kind creations, tailor-made for each patient,” and the agency’s long-promised regulatory guidance for such products has not materialized.
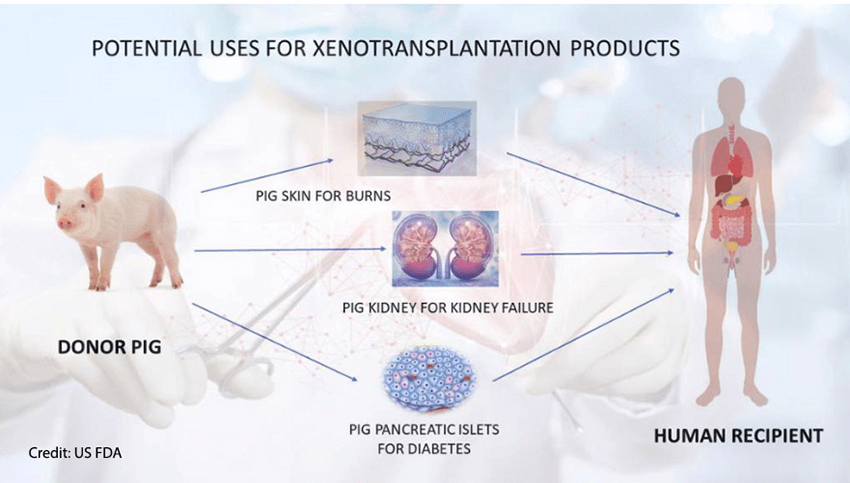
Organs from genetically modified pigs
A second approach to providing a sufficient supply of organs for transplantation is genetically engineering animals — most often, pigs (because they are an appropriate size) — so their transplanted organs will not be rejected. In effect, it uses genetic engineering to grow “humanized” tissues and organs in animals. There was a breakthrough with this approach in 2018 when scientists used gene editing to create hybrid embryos containing both human and sheep cells.
Another milestone occurred in December 2020 when the FDA “approved a first-of-its-kind intentional genomic alteration (IGA) in a line of domestic pigs” called GalSafe, which may be used for food or human therapeutics. The IGA in the animals eliminates the gene that makes α-Gal, a sugar molecule found naturally on the surface of porcine cells. It is the source of allergy in some people when they consume certain meats, and it is also involved in tissue or organ rejection after transplantation into humans. That was the first IGA in an animal approved by the FDA for both human food consumption and as a potential source for therapeutic uses.
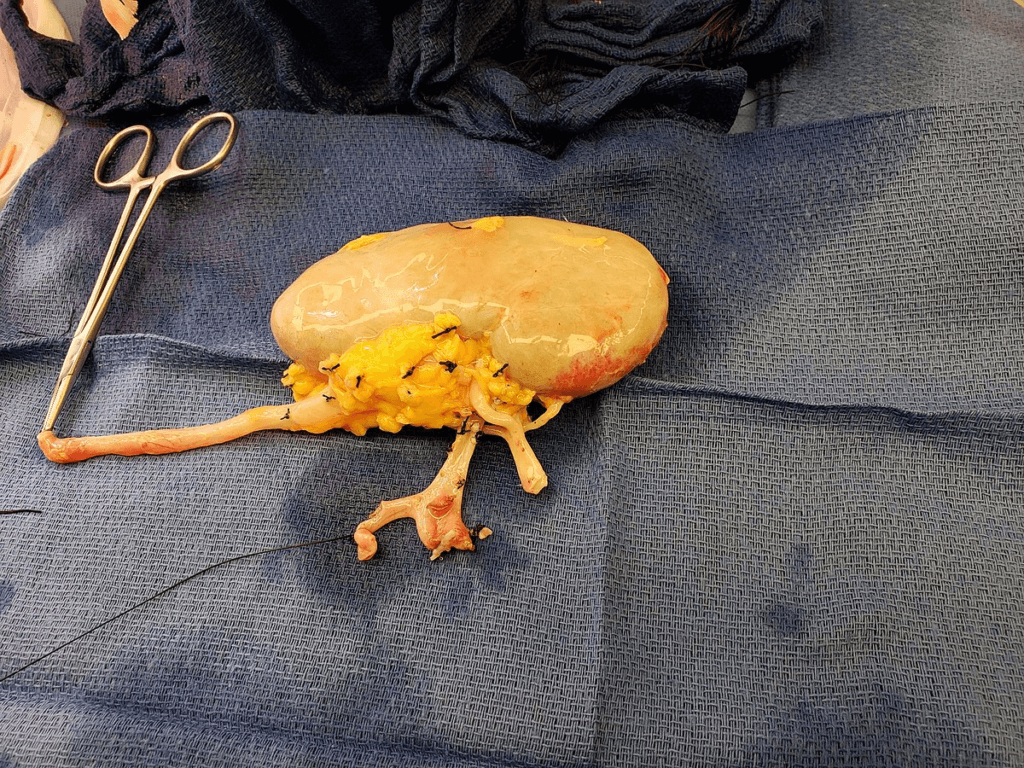
There is considerable research underway to create lines of pigs for transplantation, but there is also controversy about the extent of genetic modification necessary to both avoid rejection and ensure the absence of harmful pathogens. Two separate, very small clinical trials blazed the trail – a pig heart transplanted into a patient with terminal heart disease and a pig kidney implanted in a brain-dead patient. The heart transplant patient died two months post-transplant, and the kidneys worked well until the experiment was terminated after three days.
In March, a gene-edited pig kidney, created using "CRISPR-Cas9" technology, was transplanted into a living 62-year-old man. The donor pig’s genome had 69 edits. Some of the changes disabled genes in the pig that could otherwise lead to immune rejection of the organ in the human recipient. Other edits introduced human genes that promoted circulation and removed pathogenic porcine viruses. It was reported on May 12 that the patient had died; the cause was not revealed.
Around the same time as the kidney transplant, researchers transplanted the liver of a pig with three genes disabled and three human ones added to prevent immune rejection into a clinically dead patient. During the 10-day experiment, the liver produced bile, and there was no sign of immune rejection.
The low-tech policy approach
Although friends and relatives and even the occasional “good Samaritan” donor can donate kidneys, they must be given without compensation. Under section 301(a) of the National Organ Transplant Act of 1984 (NOTA), it is a federal crime for “any person to knowingly acquire, receive, or otherwise transfer any human organ for valuable consideration for use in human transplantation if the transfer affects interstate commerce.” Therefore, we propose a federal tax credit for living donors willing to save the life of a stranger. The value of the reward should be between $50,000 and $100,000, which physicians and others who endorse donor compensation believe would be sufficient to address the organ shortage. An economic analysis published in 2022 estimated that a reward of $77,000 could encourage sufficient donations to save 47,000 patients annually.
The credit would be universally available—refundable in cash for people who do not owe income tax, not phased out at high-income levels, and available under the alternative minimum tax. NOTA’s restriction on payments by organ recipients and other private individuals and organizations would not change—it would still be illegal for recipients to buy organs.
Credit: Rmarlin via CC-BY-SA-4.0
A qualified organ donation would be subject to stringent safeguards. As all donors are now, prospective compensated donors would be carefully screened for physical and emotional health. A minimum six-month waiting period before the donation would filter out impulsive donors and donations by financially desperate individuals seeking instant cash.
In addition to saving lives, the credit would save the government money, perhaps as much as $14 billion per year, by reducing expenditures on dialysis. Thus, donors would receive financial compensation from the government for contributing to the public good and bearing the risk of a surgical operation to remove the organ.
This would be a compassionate and pragmatic policy. Moreover, it could be implemented immediately, rapidly clearing much of the backlog of Americans waiting for organs in advance of the longer-term high-tech approaches.
The organ shortage kills thousands of Americans every year. We must do all we can to alleviate it now.
Henry Miller, a physician and molecular biologist, is the Glenn Swogger Distinguished Fellow at the American Council on Science and Health. He was the founding director of the FDA’s Office of Biotechnology. Follow Henry on Twitter @henryimiller
Sally Satel, a psychiatrist and senior fellow at the American Enterprise Institute, is a kidney recipient. She and economist Alan Viard developed the tax proposal in depth. Follow Sally on Twitter @slsatel
An earlier version of this article previously appeared on the Genetic Literacy Project on February 23, 2024.