A breakthrough, almost decade-long study of a spray vaccine offers promise for hundreds of millions of women who suffer from urinary tract infections (UTIs) over their lifetimes.
The vaccine, called Uromune, was developed by Immunotek, a Spanish-based pharmaceutical company. It has been approved for use in two countries, the Dominican Republic and Mexico, and is under review for approval in Canada. It is also available under special-access conditions in 26 countries, but not the US.
The vaccine, called MV140, is administered with two sprays of a pineapple-flavored suspension under the tongue every day for three months. The suspension contains four species of inactivated bacteria. Although researchers have previously studied MV140’s short-term safety and effectiveness, the first long-term follow-up study to report globally was presented in April at the European Association of Urology (EAU) Congress in Paris.
“Nine years after first receiving this new UTI vaccine, around half of the participants remained infection-free,” said Bob Yang, consultant urologist at the UK’s Royal Berkshire NHS Foundation Trust, which co-led the research. All participants had a history of recurrent UTIs.
After nine years, 54% of participants did not develop a UTI since taking the vaccine. On average, study subjects went four-and-a-half years without getting an infection. Those who did develop a UTI tended to suffer only minor symptoms.
Most recurrent UTIs now require short-term antibiotic treatment, but the effectiveness of these drugs is waning as antibiotic-resistant infections increase.
The revolutionary vaccine could dramatically advance women’s healthcare globally, saving money, hospital visits, and lives, and enhancing quality of life. Although men are afflicted with UTIs with lower frequency and less intensity, the study showed that they could also benefit from the spray vaccine.
Global health challenge
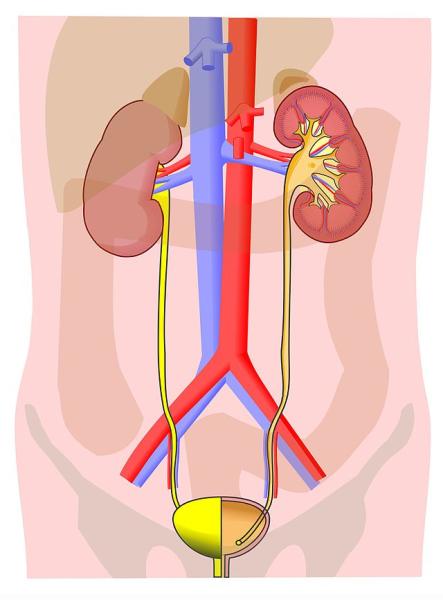
Urinary tract infections are common, especially among women. Approximately 60 percent of all women will develop a UTI at some point in their lifetime, and more than 25 percent develop recurrent UTIs, defined as three or more occurrences in one year or two or more episodes in six months.
UTIs are associated with considerable morbidity and mortality, with as many as four percent of hospitalized patients dying. In the US, women with a UTI have impaired activity in daily life, worse health-related quality of life, reduced workplace productivity, increased use of healthcare resources, and increased costs.
Added to these objective measures are the pain and frustration of having to wait days for the results of antibiotic testing and the frequent ineffectiveness of antibiotics, which are the current standard treatment for the condition. Many women are left to figure out how to manage the pain and discomfort on their own.
UTIs are also a drag on the healthcare system. Physician visits for UTIs account for up to 6 percent of all healthcare visits (roughly seven million visits) in the US and are estimated to cost up to $1.6 billion annually.
Although much has been written about UTIs in the medical literature and the lay press, women seeking help for the problem often find that urologists and primary care physicians have little to offer besides antibiotics. They are told to drink adequately and relax their pelvic muscles to wash out the bacteria. While this may offer a modicum of help in avoiding recurrence, it’s far from a cure. Moreover, antibiotics are toxic to beneficial microorganisms as well as pathogens and can have gastrointestinal and other side effects.
Vast amounts of antibiotics are being used to treat recurrent UTIs, with some women being on prophylactic antibiotics for six months or longer. That contributes to the worldwide problem of antimicrobial resistance. In addition, even after the appropriate course of treatment, in a proportion of women, the infection returns, requiring multiple rounds of sometimes ineffective antibiotics.
The reason for the persistence of the infections is poorly understood, but research suggests that recurrent UTIs may be caused by colonies of bacteria surviving in the bladder wall that are resistant to the drugs. In addition, the infection appears to trigger immune responses, including both acute and chronic inflammation, that may predispose to recurrent infections.
Beyond antibiotics, intravaginal estrogen preparations (for postmenopausal women) and probiotics (Lactobacilli) are sometimes prescribed, but clinicians have little else to offer those with recurrent UTIs. Frequently, they direct patients to take other products for which there is little high-quality scientific evidence of effectiveness.
Given the problem of antimicrobial resistance and the deleterious effects of antibiotics on beneficial microflora, urologists have called for new approaches to treating recurrent UTIs, including immunomodulatory interventions.
MV140 vaccine study results
The study, whose results were reported in April, included 89 patients (72 women and 17 men) with recurrent UTIs who were given the vaccine and followed initially for 12 months. Follow-up after 9 years involved consulting electronic health records and recontacting participants to update information on UTIs and side effects.
The significance of the study’s results is their suggestion that the effects of the vaccine are long-lasting. In addition, they align with the results of a larger study — a randomized, double-blind, placebo-controlled clinical trial published in the New England Journal of Medicine Evidence in January 2022. That study included 240 women 18 to 75 years of age from Spain and the UK with recurrent UTIs. They each received MV140 for three or six months or placebo for six months. The primary endpoint was the number of UTIs in the nine months following three months of intervention. A secondary endpoint was the number of UTIs following six months of intervention.
The results were impressive. Among women in the placebo group, the median number of UTIs was 3.0, compared to zero in both groups receiving MV140, a difference that was highly statistically significant. Among women who received the placebo, 25 percent were free of UTIs compared with 56 percent and 58 percent of those who received the oral vaccine for 3 and 6 months, respectively.
The authors concluded: “In this controlled trial… MV140 showed promising clinical efficacy in reducing recurrent UTIs in women suffering from this condition. Adverse effects were not clinically limiting.” Data on over 20,000 patients who received the vaccine in special access programs provided further evidence of a favorable safety profile.
In a May 2023 interview, J. Curtis Nickel, one of the authors of the NEJM Evidence paper and professor of urology at Queen’s University in Kingston, Ontario, sketched out how he expects licensing of the MV140 vaccine, under the commercial name Uromune, to proceed. It is available in many countries in Europe, the UK, Australia and New Zealand under special access programs in which physicians must fill out forms stipulating that antibiotics aren’t working in these patients.
North America availability
In March 2022, the Canadian healthcare company Red Leaf Medical submitted an application to Health Canada for the licensing of Uromune. The application is still under review. Citing what Dr. Nickel called “the huge unmet need,” he hopes that regulators will give conditional approval to the vaccine for use by prescription in Canada for women with recurrent UTIs, based on the half dozen studies that have been done in Europe and the New England Journal of Medicine Evidence article described above.
Dr. Nickel expects Uromune's approval to take longer in the US, where the Food and Drug Administration has more rigid rules for vaccine approval. Another large randomized clinical trial likely will be required before the vaccine receives FDA approval.
Is this necessary?
We think not. Dr. Henry Miller, a co-author of this article, is a 15-year veteran of the FDA, including as a Medical Reviewer, Special Assistant to the Commissioner, and founding director of the Office of Biotechnology, and he and others believe this is unnecessary. Given the favorable safety and efficacy profile of Uromune and the clear mechanism of action, it should be approved based on existing evidence, perhaps with the requirement that the sponsor conduct a post-marketing (Phase 4) trial.
There is a significant unmet medical need for an effective non-antibiotic prophylactic intervention for recurrent UTIs. The sublingual MV140 vaccine provides an effective treatment option for women who have been suffering and addresses the problem of widespread antibiotic overuse.
Note: An earlier version of this article was published by the Genetic Literacy Project.
Geoffrey C. Kabat is a cancer epidemiologist who has done research on a wide variety of exposures, in relation to the risk of specific cancers, including electromagnetic fields, pesticides, smoking, obesity, hormones, and diet. He is the author, most recently, of Getting Risk Right: Understanding the Science of Elusive Health Risks. Find Geoffrey on X @GeoKabat
Henry I. Miller, a physician and molecular biologist, is the Glenn Swogger Distinguished Fellow at the American Council on Science and Health. He was the founding director of the FDA’s Office of Biotechnology. Find Henry on X @HenryIMiller