
Eric Boodman, in Part 4 of the series Coercive Care, presents a study raising the specter of “the denial of reproductive autonomy for people with sickle cell disease.” Mr. Boodman “focuses on narrative features, exploring the startling ways that science and medicine affect people's lives,” so while we may all agree upon the statistical dots he cites, we may take exception to the resulting narrative.
Some Necessary Context
Tubal ligation or tubal sterilization is the most common form of contraception in the US, in part because it is non-hormonal, highly effective, and essentially one-and-done. According to the National Center for Health Statistics, while the choice to use contraception did not vary with education, the method did; those with lower educational levels more frequently opted for tubal ligations. Older women more regularly chose tubal ligations, and despite the study we are about to consider, race was not a factor.
Sickle cell disease (SCD) is a genetic blood disorder that affects approximately 100,000 Americans, most frequently those identifying as Black. For reproductive health, SCD is of some concern.
- “SCD is associated with three to seven times increased risk of severe maternal morbidity (SMM) and 11 to 50 times increased risk for maternal mortality.”
- The safety of hormonal contraception is uncertain in SCD, where there is heightened, debilitating clot formation.
- SCD is associated with higher-risk pregnancy.
Despite these findings, genetic counseling for SCD to prevent transmission of SCD to a new generation and protect the mother from maternal morbidity and mortality has been fraught with racial concerns for decades.
“Some elements of the black community view this goal as an effort to limit the size of the black population (genocide).”
– Charles Witten, MD NEJM, 1973
Tubal Ligation (Tubal Sterilization) Postpartum
Mr. Boodman’s article is based on a study funded and subsequently cited by STAT, which seeks to identify whether there are disparities in postpartum tubal ligations in women with SCD.
The data came from the 2012-2019 National Inpatient Sample, a retrospective federal dataset covering 97% of the US population and their inpatient admissions. Among women aged 12 to 55, it captured approximately 29 million inpatient deliveries during that period – 18,860 involving women with SCD and 2,945 involving women with cystic fibrosis (CF). CF patients acted as the control because it, too, is an autosomal recessive disease transmitted to the child when both parents are affected, and these women have similar issues with infertility and high-risk pregnancies, resulting in severe maternal mortality. Conveniently enough, SCD predominately impacts Blacks, while CF predominately impacts Whites.
The primary outcome was the rate of immediate postpartum tubal ligation. The secondary outcome was intrapartum significant maternal morbidity. [1]
- Tubal ligations occurred after 88/1,000 SCD deliveries, 66/1,000 CF deliveries, and 67/1,000 non-SCD deliveries
- Multivariate analysis indicated that CF and SCD were associated with equally higher rates of tubal ligation.
- The experience of significant maternal morbidity doubled the odds of tubal ligation in women with SCD but not for women with CF
There were some variations based on hospital and geography that I have chosen not to discuss. One additional patient variable not mentioned in the study or discussed in STAT’s report is that of all the factors considered, undergoing C-section was by far the greatest driver of tubal ligation, irrespective of the presence or absence of SCD or CF [2]
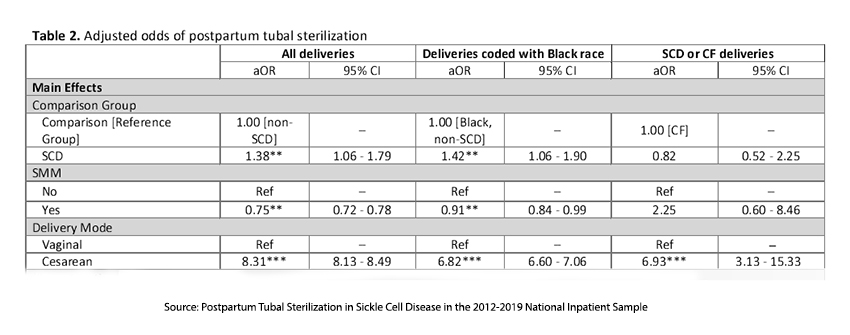
The role of genetics was addressed by comparing tubal ligation rates of women with SCD or CF who have similar, but not identical, autosomal recessive conditions. The adjusted odds of postpartum tubal
“were not different between individuals with SCD and CF. The lack of differences …suggests that the higher postpartum T.S. rates in individuals with SCD compared to those with CF are primarily driven by differences in patient and hospital characteristics between the groups.”
A previous study by the National Bureau of Economic Research reported by the N.Y. Times found, as I commented, that physician and hospital characteristics did not explain disparities in C-sections, so let us assume that this is frequently the case for tubal ligation. Are there other studies that shed light on the decision to pursue tubal ligation?
Patient Characteristics
A study in Obstetrics and Gynecology looked at a national sample of 7,600 women aged 15-44 (National Survey of Family Growth) who had undergone a tubal ligation. While they found that women with public or no insurance were more likely to undergo tubal ligation than women with private insurance, they also reported:
“After adjusting for age, insurance status, parity, income, education, marital status, and religion, African-American women were more likely than white women to undergo tubal sterilization (adjusted odds ratio 1.43)” [emphasis added]
Women with CF were 7-fold less likely to choose tubal sterilization, opting 42% of the time for hormonal treatments.
A smaller study, more focused on the “racial differences in attitudes and knowledge about sterilization,” published in Fertility and Sterility, consisted of one-on-one interviews identifying the “patient-level factors that may steer African American women toward sterilization over other contraceptive methods.”
Many of the African American women choosing tubal ligation had experienced an unintended pregnancy. The researchers suggested that these women “may develop a heightened sense of perceived fertility and/or diminished locus of control and perceive sterilization to be an effective way to gain control over their fertility.” This question of bodily autonomy might explain, equally well, the choice of tubal ligation in the face of significant maternal risk.
- African American women in the study reported more family influence on their contraceptive decisions, particularly from mothers, and had more family members who had undergone tubal ligation.
- After adjusting for sociodemographic factors, the racial difference in sterilization rates became less significant, suggesting that socioeconomic status (SES) may play a more substantial role than race in shaping responses to unintended pregnancy.
- Additionally, they noted among African American women a “greater preference to avoid a method that required insertion of a foreign object or that decreased sexual pleasure, greater misinformation about sterilization, and less awareness of IUDs…”
“These numbers can’t tell us why each sterilization took place.”
The current STAT study is based on administrative billing information. As the study’s authors note, they
“cannot capture clinical severity … [or] identify all factors that shape individual preference or clinician recommendations for postpartum T.S. [tubal sterilization].”
Given that disclaimer, much of the narrative Mr. Boodman provides are provocative questions, surrounded by a whiff of accusation. For example, having provided a quote by the study’s first author, Amy Luo, confirming the inability to conclude whether these treatment decisions were autonomous or not, he feels the need to balance that disclaimer with these quotes.
“When you look at these discrepancies, it’s much harder to claim, ‘Oh, that’s just a few folks who have bad doctors.’ You have to start thinking, what are the systemic reasons why we are seeing these kinds of disparities?”
- Kim Mutcherson, J.D., Bioethicist and Professor of Law, Rutgers University
“It’s important to celebrate that people are getting the kind of contraception that they desire. But if those differences are due to outside pressures, that’s concerning — and this study, while preliminary, does signal some potential cause for concern.”
- Kavita Arora, MD, Professor General Obstetrics and Gynecology, University of North Carolina
“You get worried, is there poor counseling? Is this still some remnant of all that reproductive coercion?”
- Nikki B. Zite, MD, MPH Professor, Vice Chair of Education and Advocacy, University of Tennessee.
In this last instance, “reproductive coercion” refers to a shameful but increasingly well-illuminated episode in US health care when eugenics resulted in the forcible sterilization of women by the State and racist bias in care taught to practitioners led to improperly compelled or inadequately explained surgical consent. After a painfully true litany of abuses, Mr. Boodman writes,
“Given all of that, the continuing variation in tubal ligation rates conjures the specter of surgeries not fully consented to.”
before pivoting again for balance,
“Then again, there are plenty of people who actively want these procedures, many of whom have to fight to get them. Coercion is hardly the only explanation for variance.”
However, he returns to his theme using the following quote.
“Maybe people are choosing to undergo this procedure because they’re unsure about their future insurance coverage, for, say, birth control pills or getting their IUD replaced.”
- Amy Luo, MS, Johns Hopkins Bloomberg School of Public Health
Both know this is conjecture, leading Mr. Boodman to disclaim, “That isn’t coercion, in the classic sense, but it isn’t free choice, either.
At the heart of Boodman's narrative is a stark question: Are the higher rates of tubal ligation among women with sickle cell disease a matter of personal autonomy, or are they the result of systemic pressures that subtly influence decision-making? The data ultimately raises more questions than answers. As much as we may hope to trace clean lines between statistics and causation, the reality is messier. The specter of coercion looms large in reproductive health, particularly today for all communities, not just those historically marginalized. Every patient navigates this delicate decision in a unique context that blends personal risk, healthcare access, and social pressure.
The study could not address those drivers. Boodman’s narrative weaves the data dots together, even beginning by affirming that the correlation is not causation, and then proceeds to suggest causation. It is unfair to the women and physicians reflected in the dots.
[1] Acute Myocardial Infarction, Aneurysm, Acute Renal Failure, Adult Respiratory Distress Syndrome, Amniotic Fluid Embolism, Cardiac Arrest / Ventricular Fibrillation, Conversion of Cardiac Rhythm, Disseminated Intravascular Coagulation, Eclampsia(Acute), Heart Failure / Arrest during Surgery or Procedure, Puerperal Cerebrovascular Disorders, Pulmonary Edema / Acute Heart Failure, Severe Anesthesia Complications, Sepsis, Shock, Air and Thrombotic Embolism, Temporary Tracheostomy, Ventilation
[2] While elective tubal ligation is considered a minimally invasive procedure, performing a tubal ligation at the time of C-section makes good sense in patient care since the surgical incision allows easy access to interrupt the Fallopian tubes. It adds a minute or two to the procedure, and because it is done in conjunction with the C-section, surgical fees are reduced by half.
Sources: Coercive Care: New analysis reveals postpartum sterilization rates are higher among US women with sickle cell STAT
Postpartum Tubal Sterilization in Sickle Cell Disease in the 2012-2019 National Inpatient Sample medRxiv DOI: 10.1101/2024.09.30.24314263



