Diabetes is a well-known risk factor for cardiovascular disease. As a clinician in assessing patients the rule of thumb, I was taught was that every year of diabetes added a year to a patient’s functional age – a 65-year-old with ten years of diabetes responded more like a 75-year-old. A paper in Diabetologia confirms the value of the heuristic, at least in their finding that a longer history of diabetes results in greater mortality.
The researchers utilized the National Diabetes Service Scheme a registry of virtually all patients with diabetes in Australia, crosslinking with mortality data. They considered outcomes for 743,709 patients with Type 2 diabetes, a median age of about 60 and 54% were men. They found that
- The earlier the age of onset of Type 2 diabetes, and therefore the longer duration, was associated with higher all-cause mortality as well as high mortality from cardiovascular disease.
- For similar durations of diabetes, say ten years, earlier onset, for a patient with onset at age 55 vs. 65, was related to even higher mortality.
- As the duration of diabetes increased, there was lower mortality from cancer.
As with any good study, the results pose more questions than answers. Why would earlier onset with equivalent duration result in higher mortality? Research suggests that dysfunction of glucose metabolism and medical problems are present, sub-clinically, before the diagnosis of diabetes. Researchers noted that patients with diabetes often are identified because other medical conditions have been identified leading to more detailed evaluation. Consistent with the belief that sub-clinical and silent medical conditions are present are other studies which have demonstrated that individuals with onset of diabetes at a younger age often are overweight, with high blood pressure and elevated cholesterol.
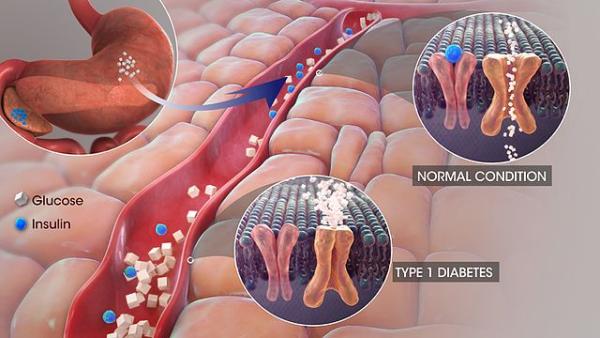
Another factor in explaining the impact of diabetes duration are the changes in the very small arteries, the microvasculature. These vessels become occluded reducing oxygenation in a subtle, diffuse way to all of our organs; often clinically manifested as failing kidney function and neuropathy, impaired perception of the signals from our nerves. Kidney dysfunction reduces our ability to control fluids; we retain more than we urinate. While this can be “managed” with drugs that facilitate urination that management is imperfect. When coupled with a failing heart, unable to efficiently pump, the fluid overload makes both conditions far more difficult to manage.
Neuropathy, a significant complication of long-standing diabetes is a source of many difficulties. We all have experienced buying new shoes and finding that they hurt our feet for the first few days when we are “breaking them in.” For a patient with diabetes, whose microvascular changes have impaired healing, the loss of pain perception can result in skin breakdown that cannot heal and can become secondarily infected or result in amputation. An even more silent form of neuropathy affects the nerves that control our heart rate, resulting in further dysfunction of the heart’s ability to pump.
The finding of lower cancer mortality in diabetes has been demonstrated in this and other studies. This too may be related to a more intense evaluation at the time of diagnosis and to better follow up. But if this were entirely the case, why the excessive cardiac mortality, are they not being screened?
The study has limitations, most importantly the lack of information on other risk factors especially smoking, weight, other associated diseases and especially glycemic control. Diabetes is a relentless disease; control is not cured. It remains unclear what is the best means of control. There is a balance between too high and too low a blood sugar. Low blood sugar is a significant source of acute complications, even death. High blood sugar results in long-term complications and death as this study has demonstrated.
Diabetes is not an isolated disease; its impact is more often manifested clinically in the interactions of glucose dysregulation with other systems, like our heart, arteries, and nerves. We have come a long way from Banting and Best [1], but we are still not as good as a normal pancreas and the other regulators of glucose metabolism.
[1] Both are Nobel Laureates for the discovery and subsequent production of insulin in the treatment of diabetes.
Source: Impact of age at diagnosis and duration of type 2 diabetes on mortality in Australia 1997–2011 Diabetologia DOI: 10.1007/s00125-018-4544-z