With the end of the government shutdown and the beginning of Congressional posturing on the rising costs of medications, the news cycle is again full of truly upsetting tales of how the cost of insulin is harming patients and their families. The first fact lost in translation is that insulin refers not to one, but several different medications and arguably is the first wonder drug that extended the quantity and quality of life in extraordinary ways. Insulin is, in a sense, collateral damage in the war of drug prices, a chimeric poster child for the best and worse in the pharmaceutical industry.
The basics
Insulin regulates the amount of glucose, sugar, in the blood, acting in opposition and collaboration with glucagon. It is released from the pancreas as the blood level of glucose rises, forcing the sugar into cells where it is turned into energy. Type I diabetes afflicts younger patients and is felt to result from infection or allergic response to one’s own islet cells, the source of insulin – these patients are dependent upon insulin. Type 2 diabetes is more of relative deficiency in insulin developing later in life in association with food choices and exercise, among other factors. While patient’s with Type 2 diabetes may take insulin, they more often take drugs that “activate my within” [1] and stimulate the production or enhance the effect of the patient’s own insulin.
Insulin’s origin story
Like penicillin, insulin has an origin story, beginning with a Canadian physician, Frederick Banting, an orthopedic surgeon who developed a line of research, suggested by another scientist, that the pancreas held the key to glucose metabolism. He formed a somewhat uneasy alliance with a skeptical physiologist, John Macleod, who supplied the laboratory, dogs and a medical student, Charles Best. Their work lead to the discovery of insulin and both Banting and Macleod were awarded the Nobel prize in medicine; Banting remains the youngest recipient of that award. A biochemist, James Collip, was brought on board to improve the yield of, and remove impurities in the insulin, which came from the pancreas of dogs; contaminants that resulted in irritation and adverse reactions in the first human patients. He was unable to convert the laboratory techniques into industrial production methods, and the Eli Lilly Corporation took over bringing insulin “to scale.”
The patent that Banting, Best, and Collip were given for the process of isolating and purifying insulin was turned over to the University of Toronto for three dollars.
“A patent was necessary to restrict manufacture of insulin to reputable pharmaceutical houses who could guarantee the purity and potency of their products. It would also prevent unscrupulous drug manufacturers from making or patenting an impotent or weakened version of this potentially dangerous drug and calling it insulin." [2]
While visiting the US, another Nobel winning physiologist, August Krogh along with his physician wife, who herself had Type 2 diabetes obtained permission to bring insulin to Scandinavia. The couple joined with an entrepreneurial pharmacist who provided the funding to create an institute to extract insulin from animal pancreases. That institute became Novo Nordisk, a global pharmaceutical giant who expend 85% of their effort in diabetes treatment.
For the next fifty years, until the early ’80s, both Eli Lilly and Novo Nordisk made insulin the old fashioned way extracting and purifying it from the pancreases of slaughtered cattle and pigs.
Insulin’s Biochemistry
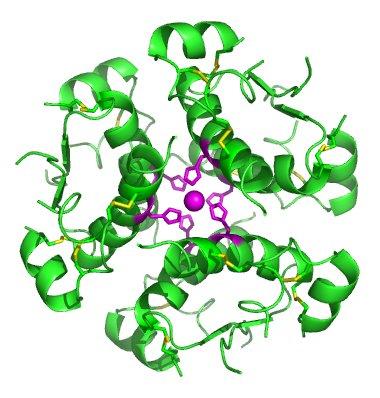
Insulin is a unique molecule, consisting of two chains of peptides linked together by three chemical bonds. Proinsulin, insulin’s precursor molecule, consists of the two chains and another segment that “carries” the Proinsulin to an area within the cell, where insulin’s two chains are linked and the carrier segment removed. These almost complete assemblies with a small remaining cap, think of it as a safety lock on a gun, are then moved into storage granules, where the “trigger lock” is removed. Insulin is then stored in groups of six, maintaining their structure while remaining inactive until called upon and released from the granules; the groups of six separating and the now fully active insulin does its thing.
Insulin is a biologic molecule with a complexity that makes it difficult to synthesize easily. Insulin was the first biologic and held that distinction for many years. Today, it has many very expensive companions used to treat other auto-immune related diseases like irritable bowel syndrome or rheumatoid arthritis - drugs that carry today’s $100,000 price tags.
Scaling production
The fact that cows, pigs and to some fish had an insulin structure very similar to ours allowed us to harvest insulin from these creatures. Eli Lilly found varying quality and quantity of insulin available from beef and porcine pancreases and did a great deal of work to not only isolate the insulin to remove impurities causing adverse reactions but to increase the yield so that insulin could be available to the growing numbers of patients in need.
By the late ’70s, the insulin gene was identified, and the first genetically modified insulin was created in 1982 using genes inserted into a bacteria or yeast. Yes, insulin that life-saving drug is the product of a GMO. Todays, industrial-scale production of insulin follows one of two pathways. DNA to form insulin’s two chains or to create proinsulin are inserted into bacteria or yeast which do the heaving lifting of synthesis, with the resulting chains or proinsulin isolated and bound together or split apart. These GMO products are considered synthetic “human” insulin.
The action of insulin maintains our blood sugar within a certain range, and merely giving a patient insulin can not mimic our body’s feedback mechanism [3] that allows careful titration to avoid too high (hyperglycemia) or too low (hypoglycemia). Synthetic human insulin eliminated some of the variation of animal-sourced insulin along with adverse effects, but it could not replicate the release of insulin by our pancreas. In an attempt to mimic those actions and to produce insulin that further reduced the adverse moments of too high and especially too low a blood sugar, scientists modified the human insulin still further, creating analogs. These slight alterations in insulin's sequence of amino acids [4] provide reliably short and long term actions. Lispro, an “analog insulin” is quickly absorbed and ultra-short acting, while glargine, another analog, is released relatively constantly over 24 hours causing no peaks or troughs.
There remains a significant controversy whether these newer and more expensive insulins produce better outcomes than the slightly older synthetics. But there is convincing evidence that for patients, these insulins are often easier to take, and compliance with medications is always an advantage.
The price of insulin
First, it should be clear that insulin as a complex biologic is more difficult to synthesize, requiring the intervention of natural means bent to our scientific will. As a biologic, its competition is not generics, but biosimilars. You can find a more significant discussion of biosimilars and generics here. In brief, biosimilars face higher regulatory hurdles and their costs while less than that of the original biologic is not nearly as large as the savings you see for a generic version of a simple chemical compound. Typically, biosimilars sell for 20% less than branded, in the world of generics that discount is usually closer to 80%.
Three companies provide the world’s insulin, the two original manufacturers, Eli Lilly and Novo Nordisk, and Sanofi, a French conglomerate, whose many acquisitions included a company making glargine, that once-a-day, slow release insulin. As with all highly concentrated, quasi-monopoly producers, the price of their products, in this case, insulin, most often rise. What new costs they incur that cause the price to rise are difficult to identify, save one: insurance companies, formularies and co-payments.
Given the controversy surrounding whether the newer and more expensive insulins produce better clinical outcomes than the slightly older synthetics insurance companies would rather pay for the cheaper medication. To “nudge” patients towards those drugs they have invented a variety of techniques; the out of pocket co-payments for the newer medications are higher and not all the newer medications may be on the formulary and available at all. In other instances, you must fail at a cheaper version before you are allowed even to consider paying those higher co-payments – a technique called step therapy. In other cases, the physician must submit reasons for choosing the more expensive medications, prior authorization.
Pharmaceutical companies fight back on both the manufacturing and price fronts. The sale of the original patent on insulin for $3 is long gone, altruism replaced by the fiduciary responsibilities of publically traded companies to show a profit to their investors. Manufacturers have dragged their feet, not providing drug samples to companies wishing to create biosimilars, they have attempted to extend their patent protection including an attempt to transfer patents to a native American tribe, whose “sovereign” rights would trump US patent law (while ingenious, the case failed).
Concerning price, the manufacturers offer discounts off “the sticker price” to both the insurance companies and directly to patients. This results in the lack of transparency in drug pricing because the price paid is unknown to all parties. If a drug is discounted by a manufacturer by 60% to the wholesaler there is no guarantee that those savings will be passed along to patients, in fact, we have good evidence that those discounts are absorbed by wholesalers and the current pharmaceutical villain, benefit managers. A drug’s sticker price is an opening bid in price negotiation; patients are involved as the source of all payments and as the collateral damage in this failed market. It has failed for a variety of reasons, but posting the sticker price, the average wholesale cost, is as helpful in buying medications as the manufacturer’s recommended sticker price is in buying a car.
Insulin is not one drug, insulin is many drugs. It is the poster child for a medical miracle and a market failure. It tugs at our past and in some ways predicts our future.
[1] Tagline for Trulicity
[2] Insulin: Discovery and Controversy
[3] Although inroad are being made in an artificial pancreas
[4] Those changes are similar to the ones that can be accomplished by CRISPR-Cas9 technologies but were developed 30 years ago and did not have the benefit of CRISPR’s precision.