Several Medicare for All proposals are on the table. I intuitively liked one alternative, a Medicare buy-in for those age 50 to 64; moving towards a well-functioning single payer system and more incremental than Medicare for All. Trying to gather enough data to put forward a back of the envelope calculation of costs proved more difficult than I anticipated – creating guesstimations that were not as precise as the numbers appeared. But often the journey is as good as the destination so to understand the proposed changes; a qualitative view will have to suffice.
My initial intuition that Medicare for over 50 is incremental is not really true. Based on the estimated 2017 census, the addition of citizens between the age of 50 to 64 would represent more than double Medicare’s beneficiaries, covering a third of the population - so much for incremental growth.
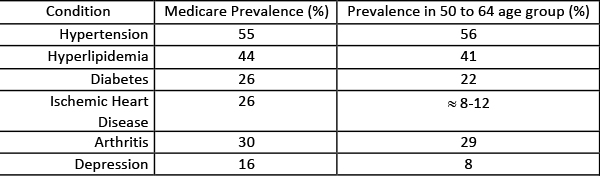
Medicare reports on the cost and prevalence of nineteen chronic conditions [1]. So how costly will it be to absorb those additional 50 to 64-year-olds? While the math remains fuzzy, the gist is clear - incorporating those beneficiaries will be as expensive. We will pick up the cost of another 14 years of chronic care and frequently the additional costs associated with the initial diagnosis. The expansion will bring more costly patients.
The current proposals are long on promises and short on funding. The plans all feature no co-payments or deductibles. But co-payments were meant to produce a bit of friction in the system, to put “skin in the game” so patients wouldn’t misuse free services. Now whether that is true or not and whether friction is the gentler term for rationed access is unclear. But if the policy thinkers believe it is helpful today, what changes in our behavior tomorrow? Deductibles clearly shift expenses, and if they to go away, costs are going to go up, how can they not?
"We have to pass the bill so that you can find out what is in it."
Speaker Pelosi’s prior statement in the healthcare arena foreshadows the debate over funding, currently addressed by hand waving and promises of more information, later. The current proposals do speak of how the funds are distributed with hospitals receiving annual budgets based on prior performance. Local budgeting is more community friendly but allows for local political chicanery – consider how local and state education budgets are aligned. Importantly, once the hospital receives its budget, it will determine the distribution of funds - a most exciting meeting to attend, as administrators play one special interest group against the other. Anyone who has sat through an operating room budget committee meeting and seen the fights of what equipment is necessary has had a preview of coming attractions. And to be a patient advocate for a moment, will patients be represented at the distribution and if so, how is there representative found?
Consider another problem, currently faced by our Medicare Advantage programs, how do you reconcile the cost of care when people leave their network, or to a hospital outside their geography? If I want to go to the Cleveland Clinic, but I live in Kansas which hospital covers the cost with their budget? Would there be an ‘ala carte’ charge creating a two-tiered system; or would we be modeling the European Union where you must convince a government agency that the care you are seeking is only available in another city?
Payer mix describes the percentage of patients having public, private or no insurance. In the Medicare for All scenarios, the private insurance, which routinely pays more than public insurance, goes away; differentially impacting hospitals and physicians. For my specialty, vascular surgery where most of the patients have Medicare, little change; for a specialty like orthopedics, with much higher percentages of patients with private insurance, we are talking significant pay cuts. Of course, since more physicians are employed by hospitals those pay cuts will be shared with other members of the health system, like the nurses and support staff.
Our healthcare system is an intricate network of relationships. Removing all private insurance will significantly perturb the equilibrium, and that might be OK, but we need to understand the possible outcomes in more than economic terms. How can we blend beneficence, justice and “doing no harm” in the proper mix? Will these changes make not only our health but our nation’s health better?
[1] Alzheimer's Disease/Dementia, Arthritis, Asthma, Atrial Fibrillation, Autism Spectrum Disorders, COPD, Cancer, Chronic Kidney Disease, Depression, Diabetes, HIV/AIDS, Heart Failure, Hepatitis, Hyperlipidemia, Hypertension, Ischemic Heart Disease, Osteoporosis, Schizophrenia, and Stroke
For those interested in more information, the Incidental Economisth has a great introduction.