While heart disease and diabetes have been touted as among the most frequent co-morbidities, as Dr. Dinerstein has written and peer-reviewed studies confirm, when the numbers are parsed, dementia and other mental health disorders claim more prominence as risk factors in the elderly.
"Among the sources of excess deaths, dementia has produced by far the most [excess deaths], more than the next two categories, diabetes, and heart disease, combined." Washington Post
But, as Dr. Dinerstein pointedly asks, why should this be so, given the lack of an obvious biologically plausible connection?
Indeed, nursing homes bear considerable responsibility for COVID-19 deaths; they are the second-highest venue (13%) of COVID-19 deaths in the US after hospitals, with deaths-at-home a distant third. But different countries report vastly different nursing home mortality rates. Deaths associated with patients in senior-care centers accounted for 40% of US COVID-19 deaths, 50% in Sweden, 62% in Ireland, and 80-85% of deaths in Canada -- compared to Singapore, where only 8% of deaths occurred in nursing homes. This intercountry variation is so large that Nature could not discount the importance of nursing home residence in their calculus of the significance of age in COVID-19-related deaths over 65.
One ready explanation for this variability is differing mixtures of the co-morbidity complexion, which renders extrapolating from one country to another for policy-planning purposes problematic. Living in tight living quarters, such as nursing homes, can also increase viral transmission. Still, there is no indication that transmissibility, a combination of infectivity and susceptibility, per se, is associated with mortality (as opposed to morbidity). Further, comorbidities affect elder vulnerability to all diseases- is there anything particularly relevant to a special COVID-19-comorbidity effect?
Notwithstanding cautionary language against the comparison of age-related statistics across countries, government policies globally included similar mandated or recommended draconian lockdowns, isolation, and visitation restriction, which were targeted to seniors living in both the community and nursing homes.
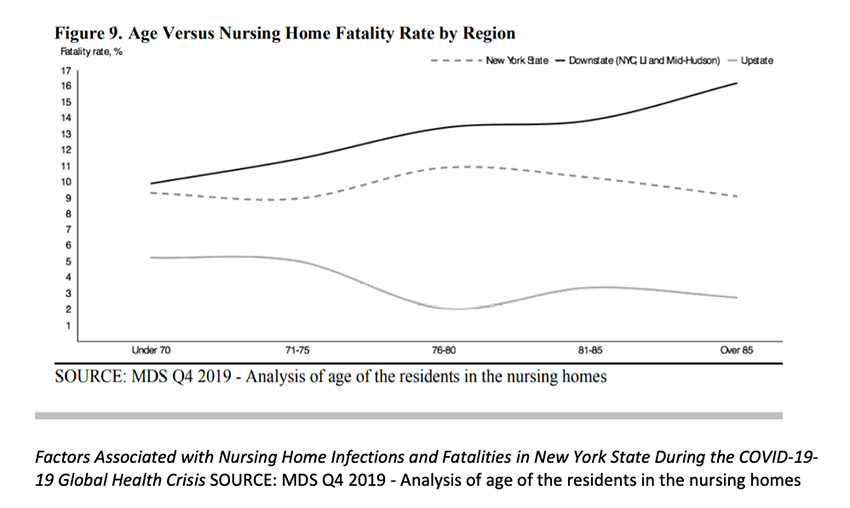
Interestingly even intra-state variations in nursing home deaths were huge. The graph provided by the New York State Department of Health compares the age of death among residents in nursing homes. Downstate nursing home residents demonstrate increasing mortality with age, but this relationship not only disappeared but reversed in upstate New York -- where nursing home residents over 70 were less likely to die than those under 70 (!). This divergence in response is a clear signal that something more than a simple and direct age and nursing-home-residence relationship is at play. The graph raises the question: which age-related co-morbidity is most significant – and is there yet another factor involved in COVID-19 deaths in nursing homes, entirely independent of age?
Another factor of note: excess dementia-related deaths also surfaced outside nursing homes. More people are simply dying of dementia and Alzheimer's this year – regardless of whether they live in nursing homes or have COVID-19. As early as June, an extra 10,000 dementia deaths were reported in England and Wales. In April alone, there were 83% more deaths than usual. In the US, similar statistics were reported, along with an explanation:
"More than 134,200 people … died from Alzheimer's and other forms of dementia since March. That is 13,200 more US deaths caused by dementia than expected, compared with previous years…People with dementia are dying not just from the virus but from the very strategy of isolation that's supposed to protect them. In recent months, doctors have reported increased falls, pulmonary infections, depression and sudden frailty in patients who had been stable for years. Social and mental stimulation are among the few tools that can slow the march of dementia . . . . Most residential care homes reported that the lack of social contact … coupled with the loss of care and stimulation provided by visitors the increased cognitive impairment and onset of depression which "caused them [the residents]… to … stop eating and drinking."
One survey revealed that “nearly 80% have seen a deterioration in the health of their residents with dementia due to lack of social contact.”
So much for our well-crafted policy of restricting contact with seniors- the approach backfired, causing excess deaths and increased mental illness - adverse events triggering bioethical and legal concerns of "therapeutic justice." (3). This may explain the relationship between age, nursing homes, and dementia. But where does race fit into the picture?
Race and Nursing Homes
Various race-related socio-economic factors have been blamed for COVID-19 morbidity, e.g., poverty, housing, and poor care. Explanations include disparities in exposure due to employment that precludes social distancing; structural racism in housing, increasing susceptibility due to crowding and fewer places to get outdoors to exercise or play; and structural racism in health care, which creates disparities in access and treatment. But while race is undoubtedly related to COVID-19deaths, its socio-economic baggage (poverty, housing, and employment) is associated with an increased infectability – and in the number of cases, not increased mortality.
However, when race and nursing home residence are combined, the mortality risk does escalate. Nursing homes with the lowest share of white residents were more than twice as likely to have COVID-19-19 cases or deaths.
"[D]eaths due to COVID-19-19 were more common among nursing homes with relatively high shares of Black or Hispanic residents" (defined in this analysis as 20% or greater).
Nursing Homes, Race, and Dementia.
The four factors: age, race, nursing home residence, and dementia at first glance, seem to be independent but additive risks, or - perhaps they are confounding and conflating one another? However, recently released statistics call these assumptions into question and raise an interesting hypothesis for further study.
- "[i]ncreasingly, residential care communities (RCCs) are becoming a source of care for older adults with Alzheimer's disease and other dementias. In 2016, 41.9% of RCC residents were diagnosed with dementia."
Indeed, this fact suggests that nursing home residence might be confounding for dementia-deaths, given that dementia, even outside nursing home residence, has been shown to be associated with COVID-19 mortality.
- 25% of nursing homes with the highest concentration of residents diagnosed with dementia (75%) were confined to one-quarter of all nursing homes – and the patient population with dementia were disproportionately located in metropolitan areas.
Metropolitan (Urban) areas are far more heavily populated with Blacks- Lower New York (including NYC) nursing home residents reported higher percentages of Black patients.
These statistics, taken in aggregate, suggest that downstate New York nursing homes housed a higher percentage of persons of color, who also happened to have dementia.
We are left with an interesting question. Are age, nursing home residence, and race all confounding for Dementia-deaths – which are exacerbated by the lockdown policy and enforced isolation? And, if so, have our lockdown policies, then, disproportionately affected and increased deaths in the portion of the Black population suffering dementia?




