“Unless the air within the ward can be kept as fresh as it is without, the patients had better be away.”
Those words of Nightingale were echoed in the Spanish Flu and COVID epidemics. As one more recent study wrote,
“A less intrusive way to minimize the risk of airborne virus transmission in schools would be to substantially increase classroom ventilation rates. To some extent, this can be achieved by increasing ventilation rates in mechanically ventilated (MV) buildings or by opening windows and doors in buildings that lack mechanical ventilation. Most of these measures were included in post-COVID opening requirements for public spaces, especially schools.”
COVID and other viral infections primarily transmitted through the air are often transmitted through poorly ventilated spaces, and there has been a concern that children, asymptomatic carriers, might well have brought infections home from school along with their homework where it was shared with other family members. Early in the pandemic, school-facilitated transmission resulted in school closure and remote learning, and subsequent observational studies have suggested that this might have been unnecessary as transmission was low. A new study in PNAS supports that conclusion for daycare centers.
The study involved ferrets, presumably because they may be easier to control than 3-year-olds and because most of us would feel that human challenge research is unethical for children. Ferrets mimic the social behavior of children in a childcare setting.
“Ferrets are curious animals that explore and play with toys and other surfaces through touch and bite behavior. They are also social animals and display considerable close-range behaviors, including chasing, biting, nuzzling, and cuddling.”
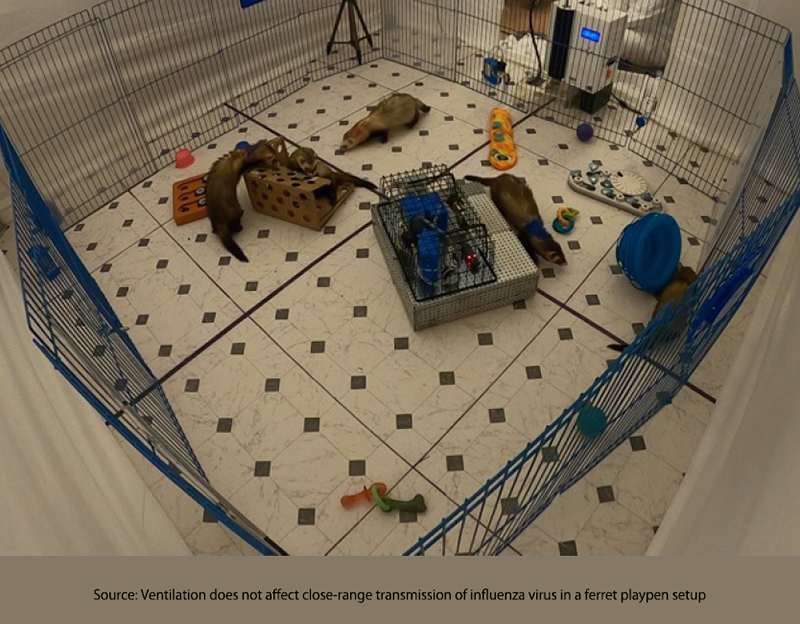 The researchers built a play area for a group of ferrets where the ventilation could be controlled, and sensors were present to measure viral infectious and non-infectious particles in the air and on surfaces. (You remember the early instructions for wiping down those cardboard boxes). A ferret infected with influenza A was allowed to have a 4-hour playdate with four uninfected ferret friends. Ventilation was set at 1.3 turnovers per hour, as found in schools, and at 23 turnovers per hour, which exceeds hospital requirements. [1]
The researchers built a play area for a group of ferrets where the ventilation could be controlled, and sensors were present to measure viral infectious and non-infectious particles in the air and on surfaces. (You remember the early instructions for wiping down those cardboard boxes). A ferret infected with influenza A was allowed to have a 4-hour playdate with four uninfected ferret friends. Ventilation was set at 1.3 turnovers per hour, as found in schools, and at 23 turnovers per hour, which exceeds hospital requirements. [1]
- Close proximity, like that found in childcare centers or our homes, resulted in transmission of the infection to the uninfected – in 58% of the cases involving low ventilation and 42% in those involving high ventilation
- The ventilation rates did not “significantly affect the amount of viral RNA” in the air. While the amount of viral RNA found on surfaces was far less than in the air, consistent with surface contamination being a minor transmitter of this respiratory virus, ventilation rates had no significant effect on deposition.
- The play-based exposures, as measured by frequency and duration, “were not predictive of a successful transmission event.”
“In play-based settings with frequent interactions at close range and multiple transmission modes possible, ventilation may not be effective in mitigating influenza virus spread.”
A Momentary Digression – Transmission Bottlenecks
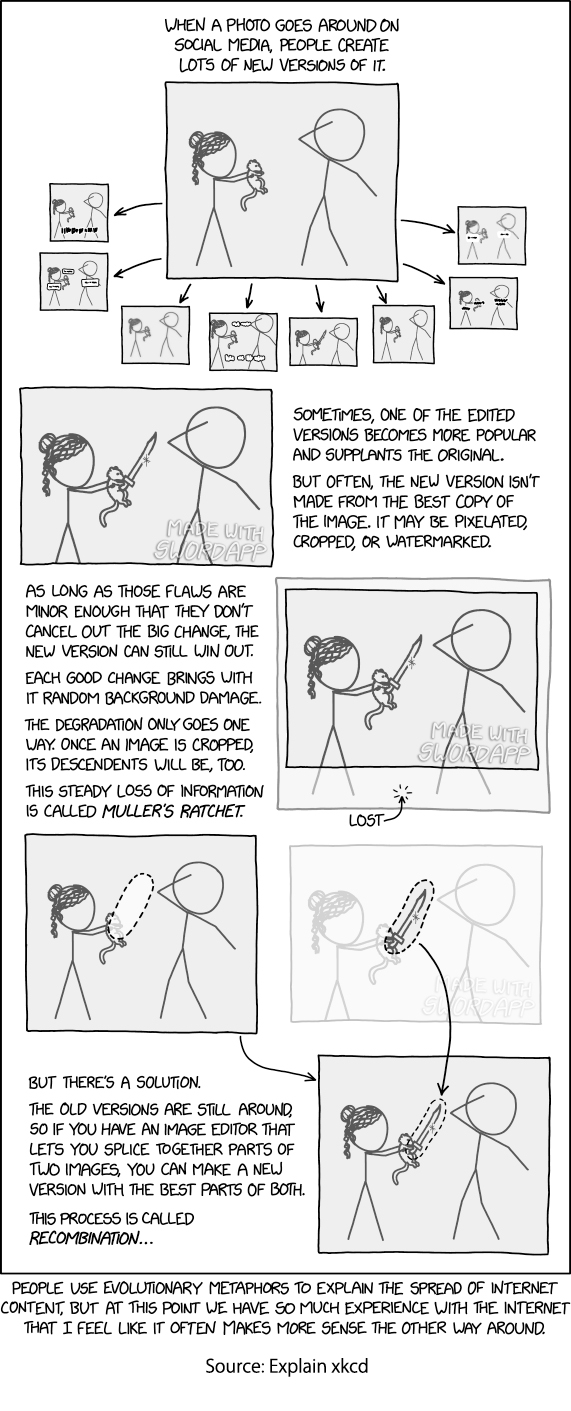
RNA viruses, we have learned, have high mutation rates, and while most may be harmful, others are beneficial, at least in the sense that they make the virus more fit for the environment it occupies. In the case of the ferret’s influenza A virus, there were a little over 4,000 genotypes with equivalent fitness, but few were transmitted to the uninfected. This rapid winnowing of possibilities to realities, the transmission bottleneck, comes from Mueller’s Ratchet – the rise of the more fit over the less fit. This is a common explanation for the loss of virulence as viruses continue reproducing in the laboratory. It seems to make common sense; the less virulent viruses maintain their host and reproduce much more than a more virulent form that kills its host. [2]
As might be expected, Mueller’s Ratchet was in full effect in this real-world study. While the infected “donor” ferret had 4000 possible genotypes, the infected ferrets had only one to three of those variants, creating the bottleneck for new variants to arise. As with other aspects of infection, altering the ventilation rates had no impact on the Ratchet.
While adequate ventilation is important, it may not be our anticipated forceful driver. At least in pre-school, where the children are less regimented and do not sit at desks at prescribed distances, increasing ventilation does not impact airborne infection transmission. The background viral particles remain little affected by increased ventilation, and it seems that the close one-on-one interaction is where transmission occurs. That makes maintaining your ”personal space” perhaps more critical than the environs. Could this be how masks work and why the data on masking, gathered based on environmental aggregates, is conflicted?
All models have caveats, and this is no exception. Ferrets are not our kids. Transmission from aerosols is mediated by gravity, and a ferret is much closer to the ground than a 3-year-old so that viral particles may hang longer in their world. There are other environmental factors, like humidity and temperature, that govern transmission, but their impact was not measured.
The notion that boosting ventilation can significantly curb viral transmission in settings like schools might be more wishful thinking than reality, especially in dynamic environments like preschools. As this ferret study highlights, the primary transmission driver seems to be close personal interactions rather than the background viral load. While ventilation plays a role in maintaining air quality, it's clear that controlling infectious spread requires a more nuanced approach that considers human behavior and interactions.
[1] Passenger aircraft turns over the cabin atmosphere every three minutes or 20 times per hour if you want a comparison. CDC recommendations during the pandemic called for two classroom turnovers per hour.
[2] Here is a graphic explanation of Mueller’s Ratchet.
Source: Ventilation does not affect close-range transmission of influenza virus in a ferret playpen setup PNAS DOI: 10.1073/pnas.2322660121