Last week, I was fortunate to hear a talk at the Population Council given by the inspiring Dr. Wafaa El-Sadr. Dr. El-Sadr is the founder of International Center for AIDS Care and Treatment Programs (ICAP) at the Columbia University Mailman School of Public Health and an expert on global HIV prevention and treatment.
She touched on many aspects of HIV infection, giving both a global and historical perspective that should inform our thinking as we approach the future. One point that she made was an idea that I had not heard before, and struck me largely both for its simplicity and its innovation.
The idea is that HIV treatment is HIV prevention.
And, that is a novel way to think about HIV at a time when creative ways of thinking are what we need. We have been waiting for an HIV vaccine for over thirty years and, although hopes are high that one will exist one day, we have to proceed with the tools that are in our arsenal at the moment.
The idea of treatment as prevention (TasP) came about, in large part, after a seminal study was published in the New England Journal of Medicine entitled "Prevention of HIV-1 Infection with Early Antiretroviral Therapy." This study looked at 1763 couples in which one person was HIV+ and the other HIV-, and saw a drastic reduction in the amount of HIV transmissions in the couples where early initiation of ART was started (96%,) when compared with delayed therapy.
That striking result is explained by the fact that when an HIV+ person takes antiretrovirals (ART,) the total number of active viruses in their body goes down. This is because of how ART works. It is designed to block HIV from replicating in the body by interfering with the process of a virus entering into a new cell and making more viruses. So, when ART is taken regularly and properly, the result is fewer viruses in the blood.
In order for HIV to be infectious, there needs to be a certain number of viruses in the blood stream. That number is not known exactly, but, it is safe to say that the more viruses are in the blood stream the more infectious a person is. The same is true on the other side of the spectrum. Fewer viruses - less infectious. To take it even farther, once an HIV+ person gets below a certain level of viruses in the blood, they become (almost) non-infectious. They do not become HIV- at this point - the HIV infection is still there. But, the likelihood that they could pass it on is incredibly low.
And, that is why treatment is prevention.
Although this approach would reduce transmission dramatically, it would not erase HIV from the population or end the epidemic.
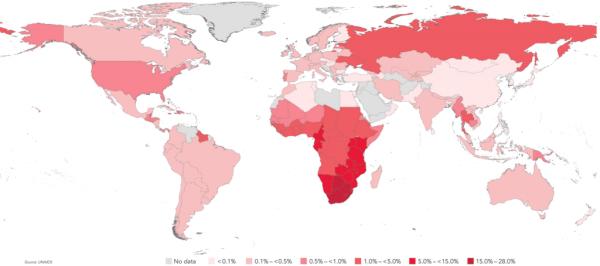
But, the epidemic is still raging and the virus is still spreading. And, the epidemic takes different forms in different areas of the world due to the varying ways that the virus is transmitted. For example, in North America, the epidemic largely affects men who have sex with other men. In Russia, it consists mostly of IV drug users. In Africa, the epidemic largely targets young women and in Southeast Asia - sex workers.
So, when faced with questions of clean needles versus condoms, voluntary medical male circumcision (VMMC) versus pre-exposure prophylaxis (PrEP) - the issues are so vast and complicated, they seem insurmountable. And, that is exactly why 'treatment as prevention' is an idea that we should get behind. Because, whether you a young woman in South Africa or a drug user in Russia, if the people that you are interacting with are receiving treatment, your chance of contracting HIV is far less likely.
Although the number of people receiving ART is increasing with each year (as shown in the graph below,) we will have to make bigger strides in making ART accessible to the most vulnerable populations in order to withness the promise of 'treatment as prevention,' - that we could, after 35 years, stop HIV transmissions and save the next generation from the nightmare of HIV.
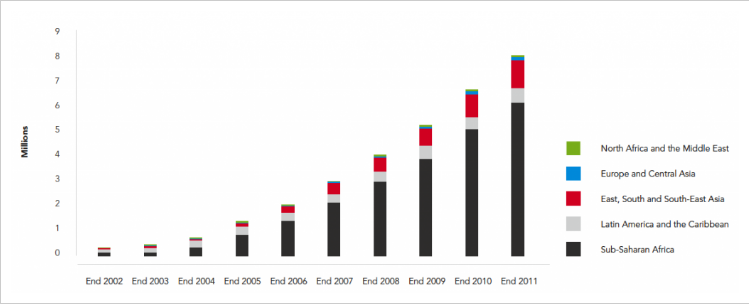
Number of people receiving antiretroviral therapy in low- and middle-income countries, by region, 2002-2011 – UNAIDS (2012) (Source: https://ourworldindata.org/hiv-aids)
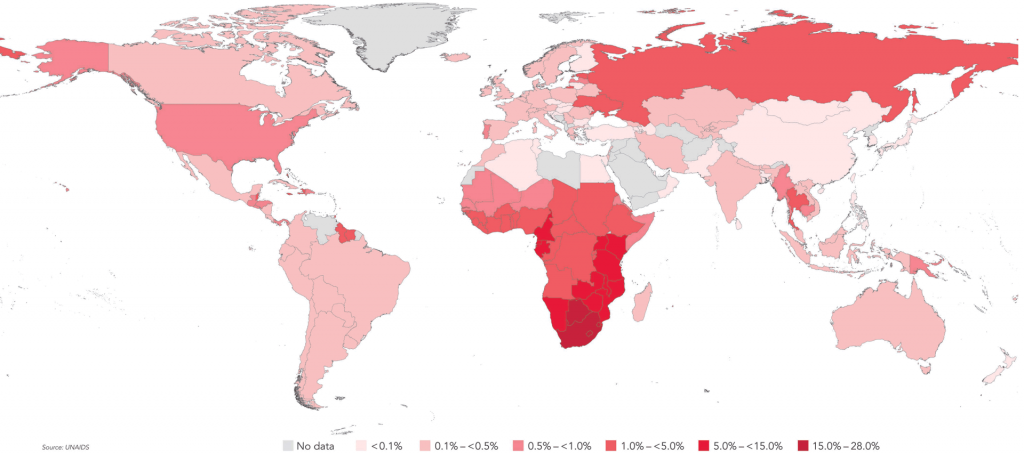
World map of HIV prevalence, 2009 – UNAID (Source: https://ourworldindata.org/hiv-aids)



