It's pretty common knowledge that obesity increases the chance that a woman will develop breast cancer, and how her excess adiposity is distributed on her body can be a clue to her risk. A new study from China increases our understanding of one possible mechanism by which this can occur.
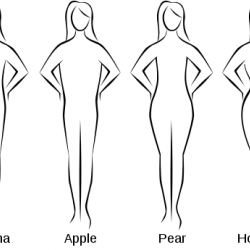
First, some words about body shapes. Most men tend to be "apples" in that they carry most of their weight above the waist. Most women, on the other hand, are "pears", carrying more of their weight in the hips and thighs, as shown in the figure above. However, some women are more like apples, and their weight is distributed more like that of men. And if apples and pears become obese, these differences are accentuated. An apple will have a higher ratio of waist to hip circumference than will a pear, given the same degree of obesity.
Dr. Zhigang Yu from the Second Hospital of Shandong University, Shandong Province, People's Republic of China and colleagues conducted a case-control study (1) of women newly diagnosed with breast cancer and their report was published in The Oncologist. The investigators noted that breast cancer is the most common cause of cancer-related deaths in Chinese women, and that its incidence has increased over the previous 20 years, and thus more clarity about the related risk factors has become more important.
The breast tumors of about 1,300 women in the study had been identified with respect to the presence or absence of receptors for estrogen and progesterone (ER+/PR+ would mean that the tumor carried receptors for both hormones, for example). They ranged from 20 to 70 years of age, and over half were between 45 and 55 years old. Further, 2/3 of the controls and about 63 percent of the cases were premenopausal. There were also about 1,300 controls.
The investigators examined the association between body size-related characteristics such as body mass index (BMI) and waist-hip ratios (WHR) and breast cancer risk for women with different hormone receptor status. They found that both BMI (as an index of overall obesity) and WHR had a positive association with risk of breast cancer. However, depending on the hormone status, the relationship between size indicators and breast cancer risk varied.
There was a significant association between BMI and risk of breast cancer — but only for women whose tumors were ER+/PR+, and for premenopausal women. WHR, on the other hand was only significantly associated with ER-/PR- status, and this latter result was independent of menopausal status.
Mechanisms responsible for the differences in the effects of overall and central obesity are not clear, the authors stated. They did note that the type of obesity a woman presents with may provide a clue to the type of treatment that would be appropriate — which could differ with respect to the receptor status and menopausal status of the woman.
This study adds to our understanding of the interactions between body size and shape and the risk of breast cancer, and in particular in relation to Asian women who have been underrepresented in other studies.
1) A case-control study is an epidemiological study that compares the effect of particular factors on the risk of disease in people with a condition of interest (in this case, breast cancer) with the risk of disease in people without those factors (the controls). These are retrospective studies, and an important limitation is the degree to which the cases and controls are matched — e.g. by age and other demographic factors as well as with the presence or absence of other conditions. They cannot be assumed to prove causation.
