Sometimes you run across an article you just have to comment upon; today is that day. Two physicians from Cleveland Clinic write almost breathlessly about how artificial intelligence will revolutionize the treatment of back pain – a highly remunerative area to physicians that has no one ascendant, best treatment regimen. (Unless you consider trying simple treatments first before proceeding to complex and invasive procedures a regimen) What is so troubling, at least to me, about the vaporware they are peddling is both their confidence in its application, and the way cost pervades their view.
The authors rightly point out, that there is a great deal of variation in who and how spine problems, i.e., back pain, are treated by the three groups of specialists that consider the spine “their organ” – orthopedists because has bones, neurosurgeons because it has nerves, and an assortment of interventional internists who can offer “less invasive” and equally efficacious care. The purported reason for the variation in care, varying levels of “experience, expertise, and pedigree… and a slew of patient-specific factors.” But all of these factors are equally true for treating many diseases where variation in treatment is not as considerable. Research suggests that physician choice especially when the best treatment is ambiguous, drives variation. And the article does contain a nugget of truth after all a blind squirrel can find a nut.
“While the spine community has a wealth of knowledge in peer-reviewed medical literature, it remains extremely difficult, if not impossible, for the practicing physician or surgeon to reconcile in real time all of the data that will ultimately determine the most cost-effective choice for a particular treatment. This can include all aspects of a specific patient, the physician’s own expertise, and all relevant financial data pertaining to the patient and the proposed care.”
Is anyone concerned about the phrase “all relevant financial data pertaining to the patient?” Does that refer to the impact of the disease on their finances or their ability to pay?
But not to worry, Cleveland Clinic is here to help us all. They are building a platform, another computer buzzword which brings to mind the image of an off-shore drilling platform; wherein collecting historical data, they will more quickly and with a “higher probability” of being correct identify the decisions that will “lead to optimal patient outcomes within the most appropriate cost and reimbursement models.” Again, why bring cost and reimbursement models into the discussion; won’t we all get the same care irrespective of our ability to pay? As to the “higher probability” of better decisions, the author’s cite a 50% improvement, the current generation of AI systems are found to be as good as physicians, not necessarily better. And while 50% sounds better, we are describing a system that doesn’t even have a published proof of concept. Can an AI system provide physicians with pertinent information to make a judgment, absolutely; but who is willing to let the algorithm decide?
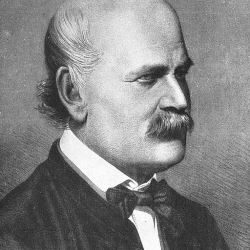
For the authors, the real value of AI, in addition to the tantalizing suggestion that care will be more “cost-efficient,” is that needless variations in care will be removed, homogenized away. To the extent that it raises sub-standard care, that is all for good. But in homogenizing variation, we inadvertently lose innovation that improves the standard. A simple example should suffice, consider how audacious a violation of the standard of care it was for Semmelweis to urge physicians to wash their hands and change out of the clothes they wore to do autopsies before seeing patients.
Source: How AI Could Help Your Bad Back Scientific American