Early on in the pandemic, the call was to flatten the curve, in order to reduce the number of cases and not overwhelm our healthcare systems. Over time, some say that has morphed into an attempt to eliminate or suppress the viral spread. A new study looks at the tradeoff.
Let's get the basics out of the way. This is a computational model — the lessons lie not in the numbers but in the relationships that form the numbers. Mitigation, our initial strategy, reduces the impact on our health system, allowing the pool of hosts to decline over time, conferring herd immunity – allowing us to return to the old normal. Sweden has taken that approach. Suppression of transmission seeks to eliminate the virus and requires additional measures as cases surge - a policy taken by South Korea, China, and Italy, among other nations. Both goals require masks, social distancing, and self-isolation.
The Model
Remember, all models are simplifications, all models are wrong, and all models may provide insights. The researchers used age-stratified data for transmission, susceptibility, and mortality but reduced complexity by creating three age groups, the young, under 25, the old, 60 or over, and the middle-aged. They used a reasonable measure of transmission, wrote the equations, and let the computer do its thing.
Suppression
This graphic displays the computational results using an effort at suppression. Don't be put off by the seeming complexity; consider the trends. Graph A shows the daily new cases without any intervention; those cases result in cumulative exposure for the population as seen in B. Using age-specific fatalities, results in the cumulative deaths depicted in C. These are the baselines.
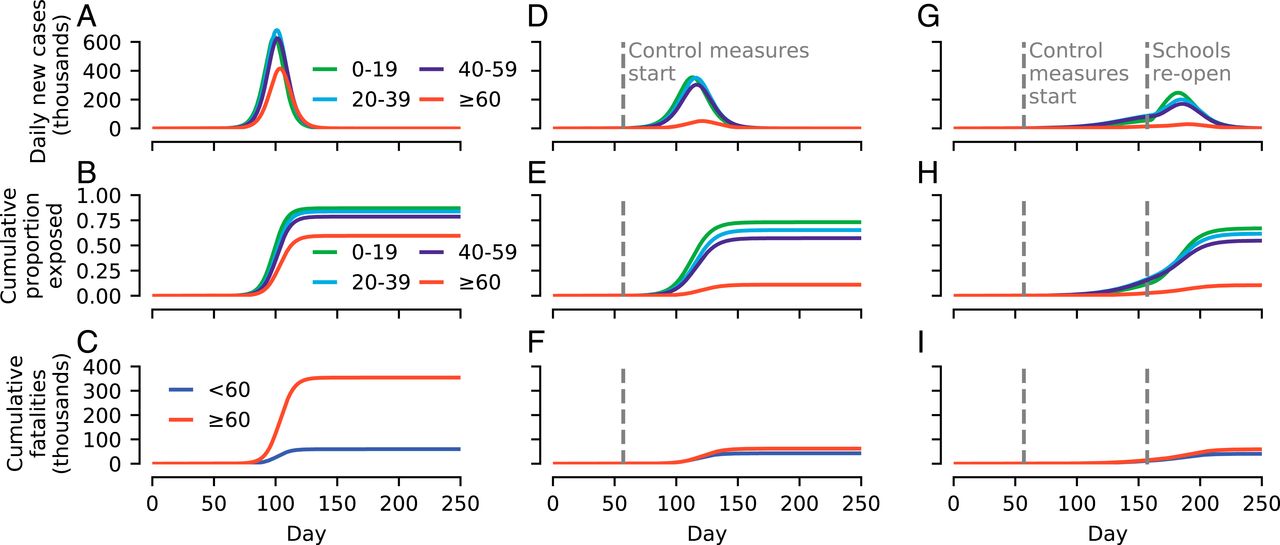
Graphs D – F show the same calculations, but older individuals socially distance [1] and symptomatic patients self-isolate [2]. The measures were enacted on day 57 when the cumulative deaths had exceeded 10,000, beginning to tax the health system. These two measures significantly reduced cases and death.
Graph G – I again show the same calculations, with the same social distancing and self-isolation but now adding school closures. The researchers re-opened schools on day 100 before the virus was fully suppressed. School closure slightly reduced cases and deaths, but any "savings" was subsequently lost by premature opening.
Suppression can be achieved but relies heavily on self-isolation. First, the researchers assume that transmission is only through symptomatic patients, even mildly so, but our data suggests that asymptomatic transmission is possible and significant. It also requires individuals to be compliant with self-isolation. Neither of these assumptions seems to be borne out in the real world. In this instance, ending the pandemic requires social distancing by every age group and all available means, shutting down schools and in-person commerce.
Mitigation
Failure to suppress the infection means that the only strategy remaining is mitigation, reducing the wave's height, lengthening the effect.
- "Social distancing by 60+-y-old individuals results in a marked reduction of the final fraction of this age group that are exposed"
- "unless both schools and workplaces are closed, additional social distancing measures do not lead to much further reduction."
- Mitigation is not entirely successful without suppression
The message is that suppression and mitigation are entwined – separating them as to policy goals is perhaps a strawman argument. The researchers offer management instead by age groups, their marker of susceptibility. In terms of lives lost, the optimum begins with the self-isolation of the over 60's and just enough social distancing of the less susceptible under 60's not to overwhelm the health systems. After immunity develops in the less susceptible portion of "the herd," self-isolation is eased among those at the most significant risk.
What to conclude?
The researcher's optimum plan remains a computer simulation. Still, it will take months to years to achieve herd immunity with continued carefully monitored lifting and imposition of social distancing and self-isolation – probably not something we can do as a society. To a certain extent, we have already instituted risk-based social distancing without government intervention. As I have noted previously, the older residents of Florida restricted their social interactions, at least based upon their cellphone GPS data, weeks before the Governor locked down the state. Or consider your pandemic bubble or posse, isn't it made up of your friends who share your sense of COVID-19's risk?
The message from "science" remains the same, social distancing and responsible self-isolation are the tools at hand that most effectively protect society's, the herd's, health. A vaccine will alter the pandemic's dynamics, significantly reducing its duration. A vaccine can mitigate and suppress COVID-19 in a way that our behavior alone cannot. The next hurdle will be finding a way to restore public trust so that vaccination can take place at a necessary scale. Consider this, in 1953 there were 35,000 cases of polio among children. Within a year of the mass vaccination program using the Salk vaccine, that number dropped to 5,600 and within four years to 161.
[1] Social distancing reduces exposure to the youngest by 90%, by 70% for those in the middle, and 50% between one another
[2] Self-isolation for symptomatic patients is 20% effective
[3] Schools reduce contact by 70% for school-age individuals and 20% for the middle age group
Source: Transmission dynamics reveal the impracticality of COVID-19 herd immunity strategies PNAS DOI:10.1073/pnas.2008087117

