Another week, another disparity of care. In this case, it's attributable to a measure known to be flawed: pulse oximetry. Does the flaw lie solely in the tool – or how it is used? Let’s take a deeper dive into the latest study of healthcare disparity.
The study, published in JAMA Network Open, is a retrospective look at patients hospitalized for COVID-19 early in the pandemic, at the height of hospitalization. Pulse oximetry (Sp02) is a quick, non-invasive way to estimate the actual oxygenation of the blood. Sa02 measures the actual level and requires drawing blood, typically from an artery in your wrist. We have good data to show that pulse oximetry may overestimate oxygenation as skin coloration darkens. But race may be a poor discriminator of skin tone. [1]
“The intensity and seasonality of ultraviolet radiation is now understood to be the primary determinant of skin color variation throughout the peoples of the world.”
Skin tone variations are found in all the racial categories of the study, making the apparent consistency of race as a category untrue, at least for the impact of skin coloration on pulse oximetry measurements.
The researchers considered three outcomes.
- Measurement error, SpO2 − SaO2.
- Unrecognized hypoxemia defined as “SaO2 levels below 88% with concurrent SpO2 between 92% and 96%.”
- Unrecognized need for treatment when “the first SaO2 in the hospitalization was below 94% despite a [within] 10-minute SpO2 of 94% or higher.”
The use of the term unrecognized need may be needlessly pejorative. Clinically, there was enough concern that the more accurate, more invasive testing, a SaO2, was obtained despite the reassurance of a “normal” pulse oximetry. In fact, among those patients having both studies, Blacks underwent those SaO2 studies the most quickly, nearly 2 hours ahead of Whites and 4 hours earlier than Hispanics.
Roughly 41,000 patients underwent SaO2 measurement during hospitalization; 8600 hundred had SaO2 and SpO2 within 10 minutes, representing the study’s dataset.
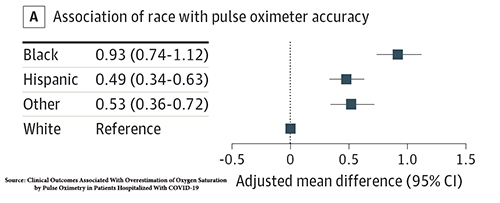 “Among Black and Hispanic patients, SpO2 consistently overestimated SaO2 at each reading.”
“Among Black and Hispanic patients, SpO2 consistently overestimated SaO2 at each reading.”
The degree of overestimation of true blood oxygenation was 1% for Blacks and for Hispanics 0.5%. Did this “modest” absolute difference in pulse oximetry readings result in unrecognized hypoxemia? Indeed, it did, most frequently for Hispanics, Blacks, other racial groups [2], and Whites. The absolute difference in unrecognized hypoxemia was 1.6% greater for Hispanics than Whites and 1.4% for Blacks vs. Whites. But there was also unrecognized hypoxemia for Whites. Pulse oximetry is not exact for any racial group.
Did these disparities result in poorer outcomes?
First, it must be acknowledged that this group of patients, with SpO2 and SaO2 measures within 10 minutes of one another, were quite ill; 46% died. For those with an initial SaO2 below 94%, the deaths rose to 54%.
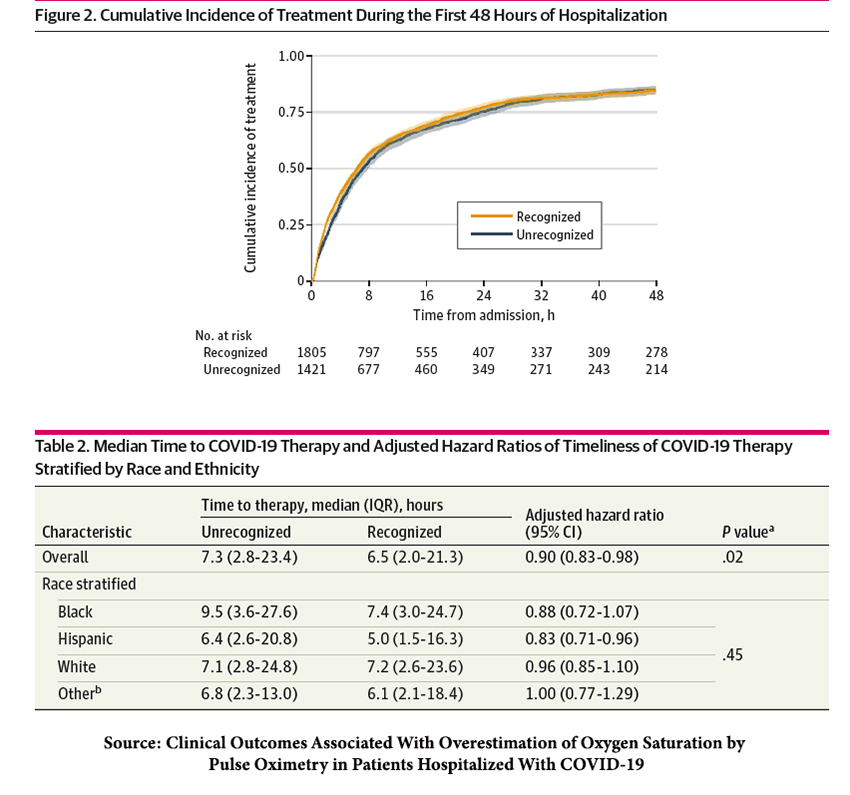 Overall, there was a 45-minute difference in the initiation of therapy between those recognized and unrecognized cases, predominantly during the first 8 hours of care. The time delays by race were not statistically significant. Moreover, time delays in treatment have many causes, including hospital census, staffing, and the queue waiting for medications from the pharmacy or treatment by respiratory therapists.
Overall, there was a 45-minute difference in the initiation of therapy between those recognized and unrecognized cases, predominantly during the first 8 hours of care. The time delays by race were not statistically significant. Moreover, time delays in treatment have many causes, including hospital census, staffing, and the queue waiting for medications from the pharmacy or treatment by respiratory therapists.
The unrecognized need for therapy reduced treatment for 10% of patients – we might presume that this fell along racial lines, but we do not know as the researchers did not report the findings. While it is statistically insignificant, those with unrecognized needs were released from the hospital a day and a half earlier and had a 16% lower in-hospital mortality.
The researchers' conclusions acknowledge the “lack of association of delayed recognition of treatment eligibility with mortality and length of stay” and that “variability in the accuracy of pulse oximeters has been previously reported, and the impact it has shown in patients of all races emphasizes the multifactorial nature of pulse oximeter accuracy, extending beyond skin pigmentation.”
Given those conclusions, one has to wonder why MedPage’s and New York Times' headlines were, respectively
“Pulse Oximetry Inaccuracies Delayed COVID-19 Treatment — Black patients more likely to have an unrecognized need for therapy versus white patients.”
“Faulty Oxygen Readings Delayed Care to Black and Hispanic Covid Patients, Study Finds”
Pulse oximetry is a tool that provides clinical guidance. When physicians are aware of the limitations of their tools, they modify their behavior – witness the many instances where a more accurate and more invasive study was ordered despite reassuring pulse oximetry. Medicine, like all human endeavors, is flawed. We can do better by improving our tools or adjusting our behavior. But to continue to use race rather than skin tone in discussing pulse oximetry only invites unwarranted criticism of our “first responders” and by social gadflies looking to attract eyes and likes.
1] The Unceasing Significance of Colorism: Skin Tone Stratification in the United States Daedalus A publication of the American Academy of Arts and Sciences.
[2] A category combining Asian, Native American or Alaskan Native, Hawaiian or Pacific Islander, other, and unknown.
Source: Clinical Outcomes Associated With Overestimation of Oxygen Saturation by Pulse Oximetry in Patients Hospitalized With COVID-19 JAMA Network Open DOI: 10.1001/jamanetworkopen.2023.30856

