The pandemic’s successful expansion of pharmacists’ scope of practice to include vaccinations has given some people the idea that pharmacists can fill other gaps in primary care, like prescribing medications for our greatest comorbidity, high blood pressure, or hypertension. A new, deeply flawed analysis of the economic benefits suggests savings of money and lives.
Here’s the headline from MedPage Today
"Pharmacist Prescribing for BP Control Makes Economic Sense"
Stat’s pharmacy newsletter echoed the MedPage sentiment. Evidently, unlike the authors at MedPage Today, I read and understood the article. Sometimes, you just have to declare shenanigans, and this economic model presented in JAMA Network Open is one of those times. Let’s begin here.
“In this simulated cost-effectiveness analysis of a 5-state Markov model, 50% uptake of a pharmacist-prescribing intervention to improve blood pressure control was associated with a $1.137 trillion in cost savings and could save an estimated 30.2 million life years over 30 years.”
Do not fear the “five-state Markov model,” it is depicted at the bottom of this diagram and reflects the possible “states” of health for a patient entering the model with no cardiovascular (CV) or renal disease.
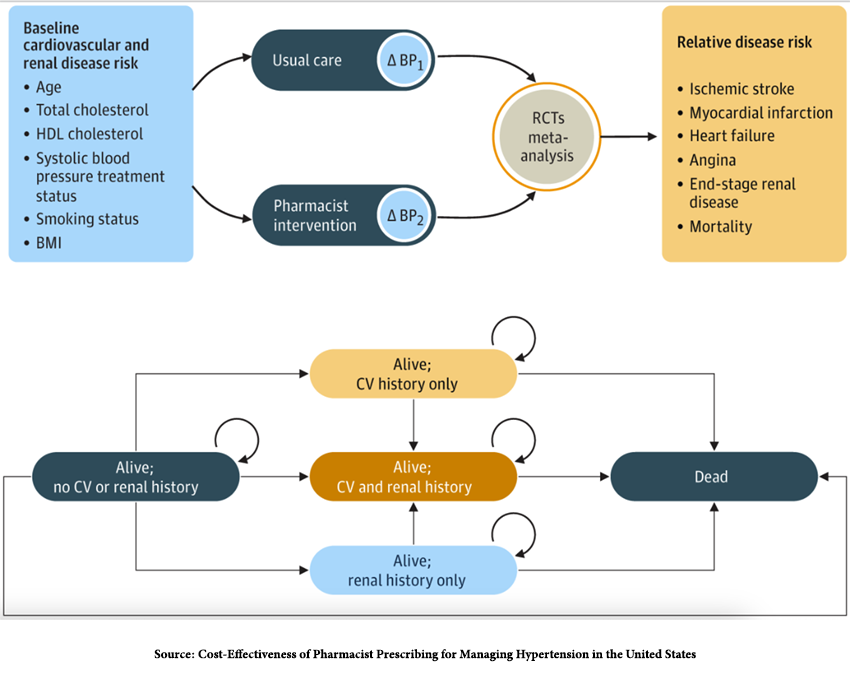
Annually, a given percentage will die, while the remaining patients will have hypertension with or without cardiovascular or renal disease. Those percentages were estimated from general population life tables, studies, and meta-analyses of cardiovascular and renal disease – standard approaches in creating these models.
The best of our real-world data tells us that hypertension impacts nearly 50% of the adult population; only about 25% of that group are treated, and overwhelmingly, >90% are treated with medications rather than lifestyle "interventions." CDC data on patient compliance with hypertension medications has an uptake of 32%, and for those most at risk, Black Americans, it drops further to 25%.
The researchers assumed in their model that pharmacists would treat 50% of adults, not the real-world 25%, and that all of these adults would be compliant with care, even though we know that isn’t the real-world case. Without using realistic data, the model's findings become increasingly fanciful.
“The conceptual model assumed that the pharmacist-prescribing intervention would reduce BP, with a resultant decreased risk of CV and kidney disease; the costs of implementing pharmacist-prescribing HTN management were thus compared with long-term cost offsets as well as health and mortality benefits resulting from this BP reduction.”
The researchers based their assumption on another study involving hypertension treated by pharmacists, and as with all studies, it comes with caveats. Briefly, this study demonstrated a 6.6 mmHg greater reduction in systolic blood pressure and a 3.2 mmHg greater reduction in diastolic blood pressure over six months when care was managed by the pharmacist in conjunction with the primary care physician.
Althought this reduction was statistically significant, its clinical value is uncertain. Pharmacists were paid $150 for their initial evaluation and $75 for each subsequent visit, with an additional group within the treatment arm receiving bonus payments for reaching target blood pressure readings. The researchers were surprised that the pharmacist-led reductions were not more significant when compared to standard care by a physician and posited that the heightened communication with the primary care physicians of BP values for the control arm, not treated by pharmacists, improved primary care results. There is also a certain irony in that the study ended early due to “funding limitations.”
The researchers’ model assumed a payment to pharmacists equivalent to that paid to physicians for this level of blood pressure monitoring, $23.10, with six visits the first year and four visits annually after that. The cost of adverse outcomes and medications were also factored into the model and extrapolated for 30 years.
For those keeping track, the model treats a larger percentage of patients with far greater success and compliance than our real-world data supports. And the “payments” to pharmacists at 1/6th of the amount provided to them when they provided care to patients.
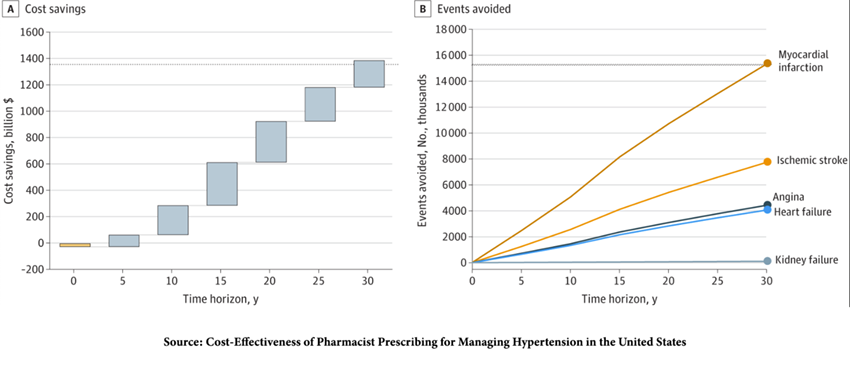
The researcher found that allowing pharmacists to prescribe hypertension therapy would result in
- 21% fewer cases of cardiovascular disease
- 0.08% fewer cases of renal disease
- $10,162/person cost savings primarily from a reduction in cardiovascular disease
- Improved life years and quality of life
“…the pharmacist-prescribing intervention was associated with both better health outcomes and lower costs…”
The researchers altered various inputs to their model to see whether these savings persisted, a process known as sensitivity analysis. Raising pharmacist payments to a more realistic $100 for the first visit and $50 for each follow-up visit indicated that the pharmacist-driven hypertension management was “still dominant,” but the actual savings were not noted. [1]
When the researchers extrapolated the model savings to treating half of the US population with hypertension, they found
… pharmacist intervention would lead to $1.137 trillion in cost savings and save 30.2 million life years over 30 years.”
Before we rush out to sign up, we should note that all of those savings in lives and costs were in comparison to no treatment at all, an unrealistic scenario. The cost savings in the real world, where pharmacists and physicians were both treating patients, would come from the cost savings associated with pharmacist-led better outcomes and lower costs. Better outcomes, in comparison to physician-led care are not presented. At best, we might assume outcomes are equivalent, but then the savings would come from the difference in payment to pharmacists vs. physicians.
Externalities
Externalities refer to factors unaccounted for in risk-benefit analysis, and those externalities make this study seriously flawed.
Approximately 6% of pharmacists work for companies employing less than 50 workers; this is the group that we can reasonably assume are self-employed; the rest of pharmacists, 94%, work for companies, so it is doubtful that the $100, $50, or $23 per visit will go directly to them instead it will be used by companies to reduce their costs. By comparison, the median hourly wage for a pharmacist is $63.82, $58.47 for a nurse practitioner, and $60.58 for a physician assistant.
A survey of pharmacists done early in pharmacists giving COVID vaccines found that 75% did not have “enough time and personnel to safely perform or meet duties.” 80% attributed their stress to “patient demands/expectations” and 76% to “the inability to practice in a patient-focused manner.” [2]
The recent walkouts by pharmacists are not about salary; they are protests about the working conditions that make it unsafe for the care they already provide. Adding hypertension management to the mix is a great idea for the bean counters but may translate into a terrible situation for those who have to do the work.
The model has deeply flawed assumptions, does not consider readily recognized externalities, and provides a comparison to no care at all. The value of the study lies solely in the headline and the way policymakers, who will never read the actual research for themselves. Instead, they will consider expanding the scope of privileges for pharmacists who are increasingly asked to abandon their primary task of dispensing and checking medications and take on responsibilities best left to primary care “providers,” – physicians and nurse practitioners.
[1] A rough guess at the change in savings would be calculated as follows. The model identifies 122 visits over 30 years at $23.10, a total of $2818.20. At the higher rates, this would amount to $6150 or a roughly 30% reduction in those savings.
[2] Six visits x 15 min = 1.5 hours of care per patient annually
122,000,000 individuals in the US with hypertension, of which 50% are treated = 63,000,000 patients
63,000,000 x 1.5 hours = 94,500,000 hours of care spread among 315,000 pharmacists = 300 hours annually. Spread out over their work week, this would reflect 16-20% of their time.
Source: Cost-Effectiveness of Pharmacist Prescribing for Managing Hypertension in the United States JAMA Network Open DOI: 10.1001/jamanetworkopen.2023.41408

