Micro- and nanoplastics, found in the plaque within our arteries, are born from the ubiquitous presence of plastics in our environment. They are raising eyebrows and heart rates among scientists and physicians, courtesy of a groundbreaking study in the New England Journal of Medicine (NEJM).
A recent study reported in the New England Journal Of Medicine (NEJM) has drawn the attention of the community of physicians and scientists researching and treating cardiovascular disease. The study aimed to investigate the presence of micro and nanoplastics (MNPs) in atherosclerotic plaque and their association with cardiovascular disease.
Ever since the phrase, "Plastics. There's a great future in plastics,” was uttered to Dustin Hoffman’s character in The Graduate, the global use of plastics has grown. We are all aware of their widespread presence and exceedingly slow degradation. Micro and nanoplastics (MNPs) are their downstream breakdown products. Microplastics range from 5 millimeters (mm) to 1 micrometer (μm) in diameter. They can originate from the fragmentation of larger plastic debris, may be intentionally manufactured for products like microbeads in cosmetics, or shed from synthetic textiles during washing. Nanoplastics from the same sources are smaller, typically measuring less than 100 nanometers (nm). For comparison, 100 nanometers is slightly smaller than the HIV, which is 120 nm in diameter. The plastics enter our bodies as we breathe and eat.
The researchers sought “to explore whether MNPs are detectable within atherosclerotic plaque and whether the burden of MNPs is associated with cardiovascular disease.” They began by collecting plaque retrieved during a surgical procedure, carotid endarterectomy. This procedure removes atherosclerotic plaque found at the bifurcation of the carotid artery in our necks, which is felt to be a cause of strokes. Specifically, they collected the plaque from individuals undergoing carotid endarterectomy that had not yet caused a stroke or stroke-like event, an indication for treatment termed asymptomatic carotid artery stenosis. [1]
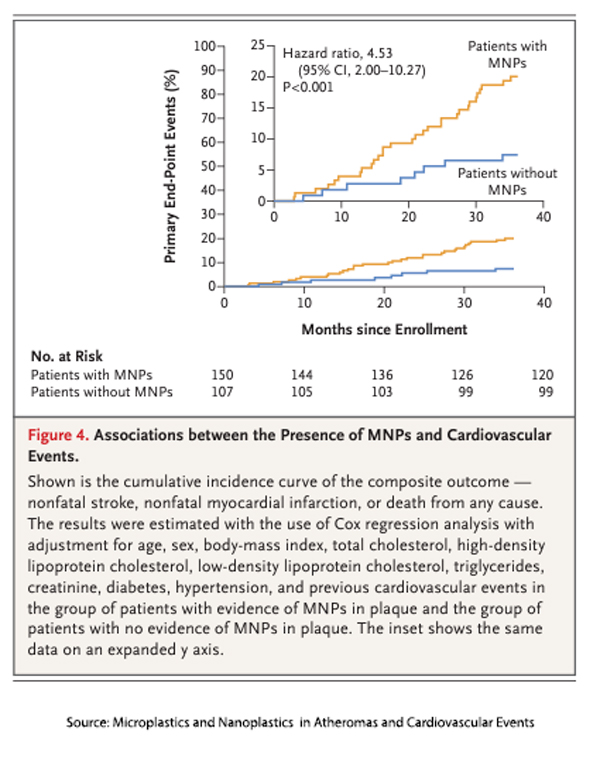 The researchers analyzed the plaques to identify MNPs and characterize their chemical makeup. The patients were categorized according to the presence or absence of MNPs and their clinical outcome – a composite endpoint of myocardial infarction, stroke, or death from any cause. After recruitment and exclusions, 257 plaques and their patients were studied for a median follow-up period of 33 months.
The researchers analyzed the plaques to identify MNPs and characterize their chemical makeup. The patients were categorized according to the presence or absence of MNPs and their clinical outcome – a composite endpoint of myocardial infarction, stroke, or death from any cause. After recruitment and exclusions, 257 plaques and their patients were studied for a median follow-up period of 33 months.
- One hundred fifty patients (58.4%) had a detectable amount of polyethylene in excised carotid plaque, and 31 of those (12.1%) had a measurable amount of polyvinyl chloride. These were the only two of the eleven MNPs researchers sought to identify in plaques, and they are the most common in our environment. Polyethylene is used in plastic bags and bottles, and polyvinyl chloride is used in pipes, insulation, and medical devices.
- Patients with MNPs tended to be younger, male, and have a higher prevalence of cardiovascular risk factors, including diabetes, elevated cholesterol, pre-existing heart disease, and smoking.
- 30 of 150 patients with MNPs had a nonfatal heart attack or stroke or died from any cause (20%); this occurred in 8 of 107 patients without MNPs (7.5%). After adjusting for those cardiovascular risk factors, patients with MNPs had a hazard ratio of 4.53, a four-fold greater risk.
- Nanoplastics seemed to accumulate more in these plaques than microplastics – the “large majority of particles detected in the current study were also below the 200-nm threshold suggested for gut and other barriers.”
Stay Calm and Carry On
This study comes with significant limitations. First, it is observational in a particular group of individuals with significant coronary artery disease risk factors. Roughly 45,000 carotid endarterectomies are performed annually in the US vs. 400,000 coronary artery bypass operations or the 900,000 coronary artery stent procedures. The participants are 5 to 11% of those much larger patients at cardiovascular risk.
“It is important to note that our results do not prove causality. The association between the presence of MNPs … and the incidence of a composite of cardiovascular disease or death outcomes may also entail the risk from exposure to other residual, unmeasured confounding variables, such as unknown exposures during the life course of the patient or, more broadly, the health status and behaviors of the patients.”
MNPs And Our Health
There can be little doubt that our air, food, and water are contaminated with MNPs and can be inhaled or ingested. There have been many studies of these particulates in “model organisms,” such as rodents and fish. MNPs might cause harm
- By their physical presence – harming cells, causing inflammation and oxidative stress.
- By their chemical presence – including the leaching and absorption of chemicals within the environment, causing reproductive and developmental toxicity or invoking an immune response.
- By their microbial passengers – introducing pathogens or disturbing our gut microbiomes.
But the key word is might; we simply do not know, as current researchers point out. The studies in model organisms involve
“high levels of MNPs are assessed — orders of magnitude beyond those observed in the present study, a factor that makes extrapolation of the relevance of preclinical findings to humans difficult.”
In the words of another researcher suggesting that MNPs could be a cardiovascular risk factor, “the clinical relevance of these findings is unknown.” The current research does not reduce our uncertainty. The accompanying editorial in the NEJM suggests physicians encourage our patients to “reduce their use of plastics, especially unnecessary single-use items.” However, microplastics are already everywhere, so this suggestion seems to have little salience.
While the association between MNPs and adverse cardiovascular events is striking, the study underscores the complexity of causality and the need for further investigation. The study serves as a poignant reminder of the intricate interplay between environmental contaminants and human health.
[1] They chose this subgroup of indications “to maximize the chances of surviving the post-procedure period and to minimize interpatient variation in plaque phenotypes.”
Source: Microplastics and Nanoplastics in Atheromas and Cardiovascular Events NEJM DOI: 10.1056/NEJMoa230982

