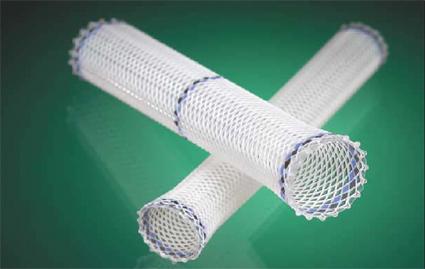
Stents are to cardiologists what hammers are to carpenters. And, with heart disease at the top of the list of causes of death both in the United States and around the world, that's a lot of nails to be knocked in.
But, those tiny wire mesh tubes may not be as useful as previously thought.
Stents are put into place to keep an otherwise clogged artery open. The idea behind inserting them is to maintain blood flow which is thought to diminish chest pain and prevent heart attacks.
But, a new study in The Lancet calls that theory into question. The study, entitled "Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial" studied 200 patients who had stable chest pain due to a blockage in a single coronary artery.
All patients were first medically optimized for six weeks with standard medications to reduce the symptoms of chest pain and the likelihood of forming blood clots. At this point, roughly half of the group (105) were treated with stents - also referred to as percutaneous coronary intervention (PCI) - and the other 95 received a placebo procedure. The placebo procedure was identical to the PCI with the exception that no stent was placed and the procedure took fewer minutes.
After a six week waiting period after either the stent placement or the placebo, the patients were put through a battery of cardiopulmonary testing to test different aspects of their heart function. They were also asked to self-report on a survey that measures health outcomes in five realms: mobility, self-care, usual activities, pain/discomfort and anxiety/depression.
Shockingly, there was no statistical difference in the group that had received the stents and the placebo group.
There have been past studies that have called the efficacy of stents into question, but focusing on the evidence (or lack thereof) that stents save lives in this same population of patients. The Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) study, published in the New England Journal of Medicine in 2007, changed the paradigm that stents save lives in this patient population. The conclusion was that placing a stent did not lead to better outcomes in the reduction of the risk of death, myocardial infarction, or other major cardiovascular events.
Even with the COURAGE study aside, stents have been long thought to alleviate pain, and with more than 500,000 stents put in each year, this study throws some questions at the bread and butter of cardiology.
It is still uncertain if these new results are going to change how cardiologists practice their medicine. More research into the importance of stents is necessary to determine if this paradigm in the world of heart disease will shift. In the meantime, if you are one of the half a million people receiving a stent this year, it may be worth a conversation with your physician to second guess if the stent is really necessary.
References: