For healthcare to improve, we need to look at the outcomes of our actions and activities, identify the source of our errors and do better. A few months ago, the Annals of Family Medicine reported on how “blame” is attributed; do we point at ourselves, others or the system?
The study was conducted based on records of the United Kingdom’s National Health Service’s National Reporting and Learning system which records all patient safety occurrences. Like many of these databases, it is required and captures much of the detail surrounding these bad outcomes – you might think of it as a paperwork version of the Transportation and Safety Boards investigations of plane and train crashes. The researchers found about 14,000 records about primary care’s poor outcomes and randomly selected about 2200 for the study [1] The defined “blame” as evidence in the free-text of these reports of judgments about “deficiency or fault by a person or people;” system failures were labeled no blame. Here is what they found:
- System failures accounted for 55% of the outcomes – there were flaws in how the healthcare system was organized.
- Forty-two percent of individuals writing these reports blamed others – termed “directed blame” by the authors.
- Two percent of the report’s authors attributed the errors to themselves, acknowledging their personal responsibility.
- The more often a poor outcome had multiple contributing factors, the more often there was directed blame.
- Poor outcomes involving judgment and interactions with patients had higher percentages of directed blame.
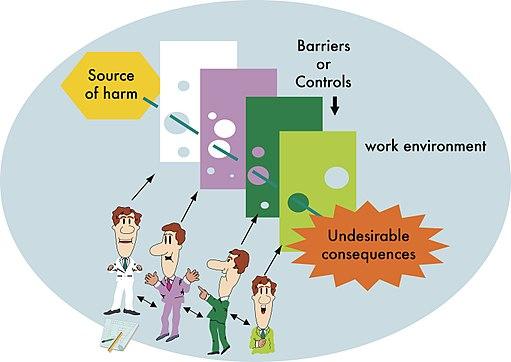
The discussion mentions a classic theory in failure analysis [2] where human error is inevitable and poor outcomes are “the result of multiple smaller errors.” More importantly, improvement comes not from deciding who failed, “but how and why the defenses failed” – what about the system lead the individual astray? Blaming others is not conducive to that kind of analysis and is often the refuge of “cover one’s own back.” It also reflects how we believe the “system” made me do it when I bear responsibility, and when someone else can be held accountable, they are bad people. Blaming others may satisfy the soul, but does little to improve care.
The article is helpful in understanding the culture of patient safety; it came to mind because of the current Congressional hearings on the opioid crisis.
“But for hours on Tuesday, executives from five drug distributor companies largely parried questions from House members and attempted to shift blame to anyone but them — to the Drug Enforcement Administration, physicians, and pharmacies, among others.
“I just want you to feel shame,” Rep. David McKinley (R-W.Va.) told the executives at one point, suggesting that financial penalties were insufficient and alluding to jail time. “So what’s the proper accountability? …What’s the punishment that fits this crime?”
Many small and large errors contributed to the opioid epidemic, and we all bear responsibility for creating the situation and for correcting our mistakes. But attribution of blame and subsequent punishment is the role of the judiciary, not Congress. Congress makes the rules. For example, the Ensuring Patient Access and Effective Drug Enforcement Act of 2016 which among other provisions made it more difficult for the DEA to bring actions against drug distributors for the egregious behavior Representative McKinley is railing against – an act passed by the unanimous consent of the House, including Representative McKinley. This behavior sounds so much like the directed blame found in the study.
Congress should investigate the bad outcomes of their legislative efforts, but this staged theater of indignation and moral high ground serves us poorly. The current Congressional hearings on the opioid crisis reflects a culture of blame rather than reflection, just like those poor healthcare outcomes reports. Improving safety doesn’t come from photo ops and sound bites on the evening news any more than it comes from nurses and physicians blaming one another. Improving safety and our legislation comes from analysis and reflection that recognizes blame as an impediment, not a response. If Congress wishes to help and use its considerable powers then it should remember President Theodore Roosevelt’s initial phrase, speak softly.
[1] The survey size was selected to be confident in the statistical analysis of their results
[2] Reason’s Swiss Cheese Model
Source: Nature of Blame in Patient Safety Incident Reports Annals of Family Medicine DOI: 10.1370/afm.2123