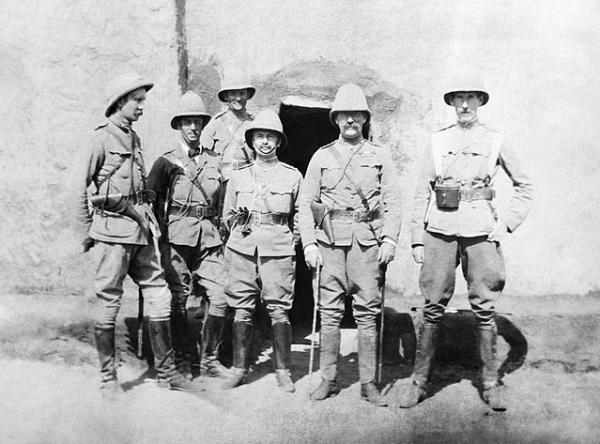
Scientism uses the cloak of quantity to explain and describe qualities, in particular qualities that lose their true meaning when reduced to a quantity. For example, how connected we feel to people is quantified as how often we communicate with them. What brought this concept to mind was in the last week, or so I have come across three studies of surgeons and their behavior that uniquely, rather than reporting on outcomes, are actual sightings of these endangered creatures interacting with others within their native habitat, the mysterious and rarely seen, operating room. So pith helmet and binoculars in hand, with Dr. Livingstone and Stanley in our hearts, what have these brave researchers found in their fleeting moments with this shy creature.
Channeling Margaret Mead and Jane Goodall
A group of ethologists, scientists who study the behavioral patterns of animals in their natural environment, sought to characterize the social behavior of surgeons. Armed with I-Pads and beliefs about gender and hierarchy A conflict from the study of the great apes, they captured about 6,300 spontaneous social interactions over the course of 200 operations characterizing the give-and-take as cooperation, conflict or neither. [1] Cooperation was the norm, reflected in 60% of utterances and while conflict was seen in about a third of operations, it was most often “social signaling,” interrupting or a curt demeanor, only 2% resulted in “physical displays” described as violent outbursts or the occasionally thrown instrument.
The most frequent communicator, the great alpha itself, the attending surgeon, murmured cooperative thoughts most frequently to their children, the surgical fellow or resident. When it came to conflict, the attending surgeon again was most vocal, two-thirds of the time, but these thoughts were directed at the creature’s helpmates, especially those lower on the researchers hierarchy of roles - the circulating nurse (26.3% of interactions) and again, the errant children, the surgical residents (20.6% of interactions) [2] They also observed several species of surgeon, finding that some, e.g., gynecologists, had the greatest cooperative communication, while others, e.g., orthopedists, had far less. The gynecologists were indeed gentler creatures with few moments of conflict; the more “temperamental” cardiothoracic surgeons were frequent communicators of conflict, 4.5% of their verbalizations rained down on the others in the room like bolts of corrective lightening.
And the gender of the attending surgeon did make a difference, but perhaps not in the way you might think. Both male and female attending surgeons acted with similar degrees of cooperation or conflict. But when the attending surgeon’s gender differed from half or more of the remaining team members, collaboration was higher and conflict less. When the attending surgeon and most of the rest of the room were female, there were more “mean girl” moments. When a male attending surgeon and males predominanted, well, “boys will be boys” – conflict rose four-fold from the predominantly female teams.” The researchers noted that
“These results are in line with the prevalence of intra-sexual competition in primate groups and the greater need for individuals in the alpha role to assert their position vis-à-vis their own rather than the other gender.”
Vocalizations varied among the participants in the room, roughly following the researcher’s proposed hierarchy, except for the always shy, anesthesiologists who spoke and was spoken to infrequently. Another problem was despite case times of a little over one hour; the researchers were unable “to continuously calculate the gender composition in the OR,” because of the frequent exchanging of one helper for another. They concluded that “team membership in the OR is intermittent and ad hoc at best. … [challenging] the assumption that ‘a team’ exists as an entity and complicates the establishment of familiarity and the formation of shared goals.”
A second, more technological approach to surgeon behavior
Perhaps to remove any observer effect or because watching surgery is in truth, pretty boring after the first few experiences, in a second study, the surgeon’s natural habitat was wired with cameras and microphones to record their behavior and utterances. This study was limited to only one surgical “family,” an attending surgeon and their children, three surgical fellows completing additional specific training in obesity or bariatric surgery. The researcher's cameras recorded one of their "rituals," a minimally invasive operation for obesity, sixty times. The researchers focused on the surgeon and fellows technical performance and their less technical chatter.
They found that fellows took longer to perform procedures than attending surgeons and had more “failures,” difficulty in carrying out a planned step of the ritual. 93% of these “failures,” were related to grasping tissue with insufficient force or errors of depth perception or orientation; failures of proprioception from working solely through instruments and video images versus actually holding tissue. [3] They were issues of skill, like a baby bird learning to fly.
The communication between these creatures, more the domain of previously mentioned ethologists, was categorized not by conflict or cooperation but as positive or negative for specific topics, e.g., situational awareness, teamwork, decision making. As the previous explorers had discovered, most of the utterances came from the attending surgeon, directed evenly between the fellows and scrub nurse. And again, most verbalizations were positive, and the attending seemed to be teaching the fellows, alternately complementing, commenting and scolding on situational awareness, leadership, communication, teamwork and decision making.
They found that the nurses also spoke amongst themselves, primarily positively but focused on their roles especially task management, situational awareness, communication, and teamwork. The researchers biggest discovery was that communication increased after a technical failure, error or it’s correction suggesting that “negative team behaviors probably preceded technical occurrences [failures], whereas more positive behaviors follow them,” especially between “the same two contributors to the team function: the surgeon and the scrub nurse.”
Diving in the data dumpster
Finally, a third study looked at how interventionalists (a surrogate marker for surgeons) negotiated the “learning curve” for Transcatheter Aortic Valve Replacement (TAVR) – a technique where the aortic valve, controlling blood flow from the heart to the aorta is replaced using catheters and wires rather than opening the chest and touching the beloved heart. Their research interest was in how a physician responds to failure, in this case the death or maiming of a patient and was based on a registry that captured all TAVR cases performed in Belgium since its introduction in 2007. [4] Would they learn and try again or sulk outside their lairs?
As with most econometric studies, most of the paper involves lots of equations explaining and weighing the components of experience, high patient volume and maintaining performance skills when long time periods separate patient interventions; what we might term less concentrated experience but economists call “human capital depreciation.” What the researchers “found” was that for any given physician, failure resulted in the next patient being 5 to 11% more likely to have a good outcome, obtaining their new valve without suffering a stroke or dying.
Divining the results of those many equations they concluded that failure’s impact on physician learning is relatively constant, you learn as much from the first death as the last. They also felt the effect of learning was short-lived, meaning that we went on to have more deaths and strokes another day; but before blaming the physician remember, patients are very clever and find many ways to ruin our plans. They concluded that the “‘learning from failure effect’ is an important source of physician learning besides the commonly identified factors such as economies of scale, learning from cumulative experience, and human capital depreciation.”
Scientism
While each of these papers sheds light on the surgical behavior, they cloak qualitative information in numbers – the essence of scientism. As a result, they continue to foster the work of Frederick Taylor [5], following in a long line of researchers with stopwatches and clipboards, believing that all of work is quantifiable and that this should be our goal.
Ask a surgeon and they can tell you that the OR is their happy place and only occasionally is it interrupted by “conflict.” When you are training younger physicians, doesn’t it make sense that a majority of your communication is with them and is both supportive and corrective? And when we operate, a good scrub nurse knows our work habits and the procedure well enough to anticipate so that we needn’t speak at all; the scrub nurse and the surgeon are in sync so that work flows. The circulating nurse also anticipates, and because they are not gloved, gowned and sterile, they are the link between the needs of the team and the world outside the OR. So should it be a surprise that most of the conversation between the team leader and the outside world is through the circulating nurse? The researchers described a hierarchy based on roles, were surgical fellows are higher up than the nursing staff. But again, ask a surgeon? Nurses are our right and left hands; the fellow is still learning and given the untoward consequences of errors, needs to be watched like a hawk. And as for econometric formulas, ask a surgeon whether they learn something when one of their patients die or suffer a significant complication; we are too competitive a group to take failure lightly. I would think that two patients dying sequentially were more a matter of random luck than a failure to learn.
Does quantification with p-values or regression equations make for a more believable truth? Or will the numbers take on their own life and return as inter-personnel metrics? “Doctor, your negative communications are surging to 8%, perhaps you should make an effort to be more understanding and ask in a positive way to keep the patient asleep and not moving.” Surgeons are doers, not scientists, sometimes the numbers keep us from seeing that reality.
[1] Cooperation was “affiliative behavior and team building” – chitchat, joking and teaching of the young by the elders. A conflict was “team-disintegrating communications” – yelling, disrespect.
[2] Evidently the researchers were not aware of the aphorism from the House of God, “Show me the medical student that only triples my work and I will kiss his feet,” which is a clearer description of the true position of the surgical fellow or resident.
[3] These are the type of errors that are corrected by “robotic” systems that employ better visualization and provide haptic feedback to the surgeon about the forces applied by their instruments.
[4] Maiming would be a significant complication, like a stroke along with renal failure or the need for a pacemaker. Only stroke demonstrated statistical significance so I guess renal failure or the need for a pacemaker is a simple fender-bender and not the head-on collision of patients dying or having a stroke.
[5] Measuring workers actions to the second, Frederick Taylor brought efficiency and productivity to the early industrial assembly lines and manufacturing and is the “father” of industrial engineering and author of The Principles of Scientific Management.
Source: Ethological observations of social behavior in the operating room Proceedings of the National Academy of Sciences DOI:10.1073/pnas.1716883115
Relationship between intraoperative non-technical performance and technical events in bariatric surgery British Journal of Surgery DOI:10.1002/bjs.10811
Learning from failure in healthcare: Dynamic panel evidence of a physician shock effect Health Economics DOI: 10.1002/hec.3668