As much as I enjoy saying “I told you so,” this case is the exception. Eating a thousand plates of crow is a small price to pay when tens of millions of lives are lost every year.
While discussing the unconventional “war” on cancer that’s currently being waged in the United States, I claimed that our ostensibly war-winning weapon—a universal cure for cancer—is very likely just a mirage. Cancer biologists are making real advances every day, so it’s not a matter of resources or brain power. Instead, it’s a function of the underlying biology. And, unfortunately, that’s something that we’re stuck with.
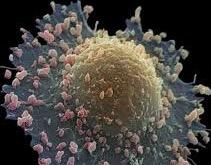
All cancers arise when DNA mutations cause cells to grow and divide uncontrollably. These mutations can either be inherited from your parents or introduced by environmental or lifestyle factors, most commonly by the sun’s UV rays, tobacco smoke, or other carcinogens. Thankfully, our immune systems almost always destroy these runaway mutants before they can cause damage. Every now and then, however, a few rogue cells will overwhelm or outflank our bodies’ defenders. The human body is a complex machine, so pockets of cells proliferating uncontrollably can wreak havoc on the systems that keep it running smoothly.
The first strike against our mythical miracle drug is a problem rooted in nomenclature. As it’s colloquially used, the term “cancer” can be misleading because it obscures the fact that cancer is not a single disease. Rather, there are hundreds, if not thousands, of distinct conditions that can be classified as cancer. “Cancer” is a blanket term that’s more akin to “viral infection” than to “influenza.” Would you expect a single drug to be able to treat HIV, Ebola, the flu, and the common cold? What about thousands of other viruses with genetic material that’s constantly changing? How is one drug supposed to account for all of that?
Also, consider how readily we separate cancer into different types: lung cancer, breast cancer, leukemia, and so on. Cancer can form in almost any tissue in the body, but it’s most common in areas where healthy cells are already rapidly dividing. For example, cancers of the skin and colon (where new cells are generated at least every couple of weeks) are much more common than cancers of the heart (where most cells stop dividing after childhood). The distinctions are particularly stark when you look at survival data: childhood leukemia and testicular cancer are often curable nowadays, but pancreatic cancer remains a death sentence. These diseases behave differently and respond to different types of treatments—they’re fundamentally different beasts.
Historically, this tissue-of-origin-based classification system has done a decent job of grouping similar cancers into distinct bins. But we’ve become increasingly aware that significant variability exists between cancers stemming from the same organ. Cancers of the brain, for example, can be sub-divided according to the cell type that went haywire: glioblastomas, meningiomas, and many more.
Even a classification system based on cell type, however, misses relationships found on the genetic level. Thanks to advances in the study of genetics and DNA sequencing technology, we’re able to identify cancers on a patient-by-patient level that share mutations and thus may present a common Achilles’ heel for treatment. This insight was first leveraged in 2017, when the cancer drug Keytruda (developed by Merck) became the first medicine to be approved to treat patients whose tumors shared a given set of genetic mutations, regardless of the tissue of origin. This new classification paradigm may turn the way we think about different cancer “types” completely upside-down, hopefully in the best way possible.
So where does that leave for our search for a universal cure? If there’s one common thread running throughout the past 50 years of research, it’s that cancer is more complex than we ever could have imagined. We haven’t actually moved backwards, per se—we’re just running hundreds of races simultaneously, each of which has a different finish line.