One of the many difficulties in treating cardiovascular disease is patient compliance with medication regimens. Many patients need to take a statin for their cholesterol, a blood pressure medication for their high blood pressure, and frequently an aspirin to reduce their risk of clotting. That can be costly, and it is difficult to remember when to and if you did take your medications. A solution has been kicking around for some time now, a low-cost single pill, a polypill that combines all of these meds. For low and middle-income countries, this may be a good approach; in fact, perhaps it is something we might consider.
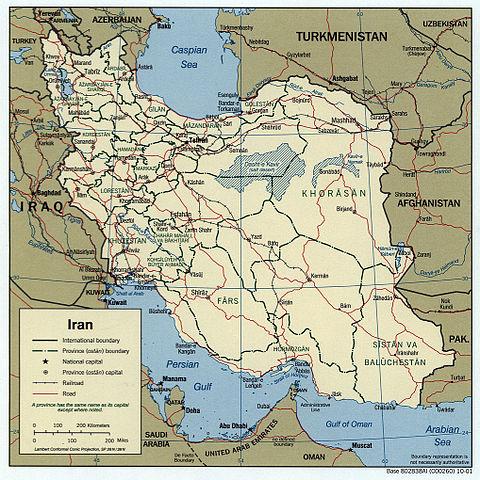
Lancet provides a report from an on-going study in Iran of just such a polypill. It has a low dose of aspirin, two blood pressure medications, and a statin [1]. The study looked at roughly 6900 individuals randomized to receive life-style education with or without the polypill. The population they were drawn from has a somewhat higher incidence of ischemic heart disease and stroke than the general population in the US and involved more individuals in rural rather than urban areas. Of the eligible individuals, half were excluded because of potential drug sensitivities or mental health concerns that would impact compliance, and another quarter were located in regions difficult to reach or declined participation. The result was a relatively compliant population with a high risk for cardiovascular disease and a low risk for adverse medication effects. Half the study population had pre-existing high blood pressure, 15% had diabetes, and about 10% had pre-existing cardiovascular disease.
Over a five-year follow-up period
- 8.8% of the education group has major cardiovascular events, 5.9% in the group given the polypill, a 33% reduction.
- When adjusting for patients already receiving cardiovascular medications, the reduction in major cardiovascular events was not as significant, 22%.
- Thirty-four people needed to be treated (NNT) to prevent one major cardiovascular event. When calculated for those at highest compliance with treatment, the NNT dropped to 20. For comparison, NNT for statins without known cardiovascular disease typically is 100.
- 14% of the patients in the polypill group developed a cough and were switched to a polypill containing a different blood pressure medication. [2] Other adverse effects were similar for both groups.
- There was no significant decline in overall mortality or non-cardiac deaths between the groups
- An initial improvement in blood pressure in the polypill group over the education alone group was lost after five years.
- The initial improvement in LDL in the polypill group over the education alone group was maintained after five years.
“…once-daily fixed-dose polypills used for a period of 5 years reduced the risk of major cardiovascular events in individuals age 50-75 years. … the polypill could reduce cardiovascular events without additional adverse events.”
The nuance
The authors speculate that based on the lack of clinical response to the two blood pressure medications, the primary benefit was derived from the aspirin and statin; raising the possibility that the polypill can be further simplified, but that will take several more years to determine. In the meantime, we have the potential of a preventative measure with few untoward side effects. In noting that major cardiovascular events were decreased to a more substantial degree (40% versus 20%) in those with no prior history of cardiovascular disease the researchers felt that the polypill had a role in primary prevention opening up its use to a larger population.
Lost in translation
Of course, the polypill may be lost in translation to high-income countries like the US.
The polypill is a population health measure, like fluoride in the water, or Vitamin D in milk. Is it possible that we can improve the results by narrowing the population to those at higher risk? And the efficacy of the treatment should give us all pause as we continue to recite the mantra of personalized, precision medicine. Sometimes a broad brush works better than one use by pointillists.
It does require that you take the medication - which is a hurdle for those individuals that are not as motivated to protect themselves from cardiovascular disease. The tradeoff may be that it doesn’t require the other hurdles burdens of preventative care, a more nutritious diet and exercise.
Pharmaceutical companies have a long history of combining two compounds, declaring them a unique combination worthy of patent protection, and removing the cost savings. According to the Financial Times, the polypill costs about $1.25/month. A rough calculation of US generic prices for the four separate pills is $40/month, the most expensive component being the enalapril at $28/month. That profitability is hard for companies to resist making the US’s continued subsidy of global medications a significant obstacle for a polypill for our population.
[1] Aspirin 81mg, hydrochlorothiazide 12.5mg, atorvastatin 20mg, and enalapril 5mg
[2] Cough is a recognized adverse effect of enalapril, which was then replaced with valsartan 40mg.
Source: Effectiveness of polypill for primary and secondary prevention of cardiovascular diseases (PolyIran): a pragmatic cluster-randomized trial Lancet DOI: 10.1016/S0140-6736(19)31791-X