Providing hospital care for those critically ill with COVID-19 has been difficult. A novel respiratory virus required novel therapeutic approaches, and while our early efforts were more art than science, hospital care today is more standardized. To better understand the morbidity associated with COVID-19, a look at care complications for those hospitalized may be informative.
The analysis looks at 75,000 adult patients, age 19 or greater, admitted for care between January and August 2020 to 302 hospitals in the UK. 86% of them had PCR confirmed COVID-19, the remaining 14% were highly suspicious cases. [1] Overall, the population being studied looks familiar; we have seen these demographics from many studies of hospitalized patients. Mean age was 71, 56% male and 81% had one or more co-morbid conditions – cardiovascular disease lead the way, followed by pulmonary and renal disease.
Overall mortality was 31.5%. 49.7% experienced a complication in their treatment. Complication, dare I say, is a complicated term. Because COVID-19 is a respiratory virus, supplemental oxygen or mechanical ventilation is not a complication, it is a treatment. The need for even more assistance in getting oxygen, extra-corporeal membrane oxygenation, or ECMO, when your blood is circulated through an “artificial lung” to enhance oxygenation, would be considered a complication. COVID-19 affects many organ systems, for it is often tough to separate the disease, like an inflammation of the heart from the virus, from a subsequent weakening of the heart’s ability to contract. And of course, we take “do no harm” seriously, so often, the term complication comes with unnecessary shame and blame.
Complications 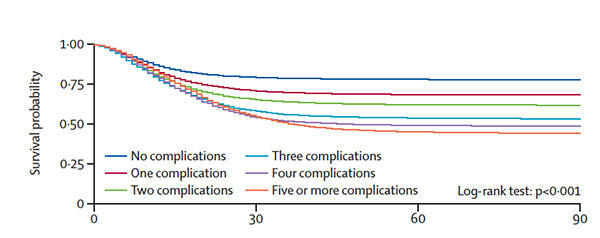
- were comparable for Whites and Southern and East Asians, as in the US, complications were more prevalent among Blacks.
- increased with age as well as co-morbidities. No surprise, those two often travel together.
- There was a direct relationship between increasing complications and death. Complications were more commonly associated with dying; 63.2% of fatalities involved one or more complications. That is not to say, survivors got off scot-free – one or more complication was noted in 43.5% of survivors.
What doesn’t kill you doesn’t make you stronger – it often leaves you maimed
Co-morbidities of organ systems already indicate problems. COVID-19 made them worse.
- Cardiac complications occurred in 19.9% of patients with pre-existing cardiac issues; half as much, only 8.9% in those without a pre-existing problem.
- Acute renal failure occurred 40% of the time in those with underlying renal disease, 21.6% in those without.
- Acute liver injury, 22.4% with underlying liver disease, 6.2% without.
Here’s the thing. Cardiovascular and complex respiratory complications (including superimposed bacterial pneumonia) were more likely to result in death, but neurologic and systemic complications were more likely to leave you “maimed.”
Many of the common complications are associated with substantial long-term morbidity
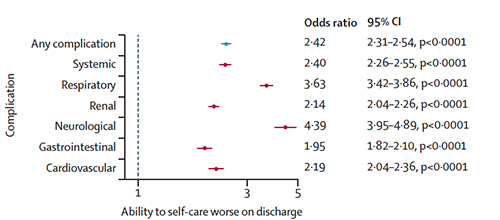 Neurologic complications were the most likely to result in a diminished quality of life; patients had poorer ability to navigate their daily lives (activities of daily living) than before becoming ill. Among the survivors, 26% had worse abilities for self-care. Before you jump to the conclusion that this primarily impacted the elderly, the loss of function was most dramatic for those under 50.
Neurologic complications were the most likely to result in a diminished quality of life; patients had poorer ability to navigate their daily lives (activities of daily living) than before becoming ill. Among the survivors, 26% had worse abilities for self-care. Before you jump to the conclusion that this primarily impacted the elderly, the loss of function was most dramatic for those under 50.
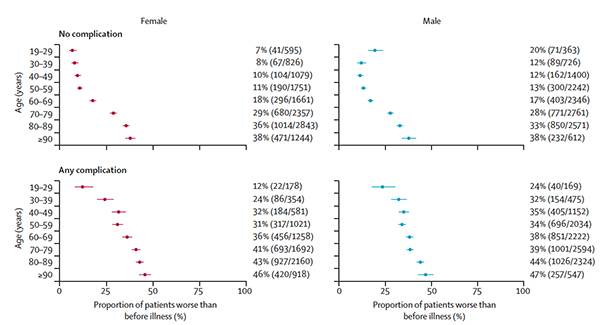 With a bit of reflection, that will make more sense. The elderly already had a number of co-morbidities and had some self-care needs. If you already are in “assisted living” or a nursing home, returning there with some new problems doesn’t change your need for assistance. But there are many under 50, held together with a bit of baling wire, grit, and some medications. It doesn’t take a great deal to uncover the underlying frailty. For them, COVID-19 is life-changing and not in a good sense.
With a bit of reflection, that will make more sense. The elderly already had a number of co-morbidities and had some self-care needs. If you already are in “assisted living” or a nursing home, returning there with some new problems doesn’t change your need for assistance. But there are many under 50, held together with a bit of baling wire, grit, and some medications. It doesn’t take a great deal to uncover the underlying frailty. For them, COVID-19 is life-changing and not in a good sense.
Vaccination reduces these concerns because vaccination dramatically reduces the severity of disease and the need for hospitalization and all that entails. The more cavalier among us point out that the worst that can happen is you die. But this study, among others, shows that this is not the case. One in 4 patients hospitalized can experience life-altering deterioration in their health and find themselves unable to get around because of a stroke or shortness of breath, or at a greater lifetime risk of requiring dialysis, or having heart problems and having to pay attention to those ads for Entresto.
[1] Complications among the “highly suspicious” were only a bit lower than among the PCR confirmed – it doesn’t materially alter the report.
Sources: Characterisation of in-hospital complications associated with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol UK: a prospective, multicentre cohort study The Lancet DOI:10.1016/S0140-6736(21)00799-6




