The New England Journal of Medicine (NEJM) is perhaps the world’s most prestigious medical journal, so it is both interesting and informative to see its editors’ compilation of what they consider its “notable articles” of the previous year. The 2022 list is impressive, especially inasmuch as the articles are from a single journal. Below are my brief summaries, with links to the original articles.
The article reported the results of an open-label (i.e., not blinded) Phase 3 study of an intravenous drug called beti-cel in adult and pediatric patients with transfusion-dependent β-thalassemia and a specific genotype. The primary endpoint was transfusion independence (i.e., a weighted average hemoglobin level of ≥9 g per deciliter without red-cell transfusions for at least one year).
Results: Treatment with beti-cel resulted in a total hemoglobin level that was high enough to enable transfusion independence in most patients with a specific (non–β0 /β0) genotype, including those younger than 12 years of age.
Comment: This is a major advance, enabling patients to avoid the inconvenience and health complications of frequent blood transfusions.
2. Biologic and Clinical Efficacy of LentiGlobin for Sickle Cell Disease
Sickle cell disease is an inherited disorder caused by a mutation leading to a single abnormal amino acid in patients’ hemoglobin molecule. Patients often have repeated blood clots, bleeding into various organs and joints, and chronic hemolytic anemia, leading to numerous complications and early death. The article reports the results of a small Phase 1–2 trial to evaluate the efficacy and safety of an intravenous gene therapy drug called LentiGlobin, which stimulates the endogenous production of the anti-sickling hemoglobin HbAT87Q.
The results were promising. “During a median follow-up of 17.3 months, median total hemoglobin increased and HbAT87Q expression was observed in most red cells. Markers of hemolysis were reduced overall. Among 25 patients who met the criteria for evaluation of vasoocclusive events, 3 had [adverse] events after infusion; there were no severe events, a reduction from the rate during the 2 years before infusion.”
Comment: This is a significant breakthrough, potentially reducing or eliminating the frequent “crises” and blood transfusions and the chronic pain experienced by patients with sickle cell disease. This advance has particular resonance for me because it was my MIT undergraduate advisor, Professor Vernon Ingram, who discovered the mutation that causes sickle-cell disease – a substitution from glutamic acid to valine at position 6 of the β-chain of hemoglobin. It provided the first confirmation that a single change in a gene could produce a single corresponding change in the protein and led to Ingram being dubbed “the father of molecular medicine.”
Because most children with tuberculosis have nonsevere disease, the investigators sought to determine whether they can be treated with shorter regimens than the currently recommended six months. The study was an open-label, parallel-group, randomized controlled trial that tested whether four months of treatment would be at least as effective as six months of treatment in children with nonsevere, symptomatic TB in sub-Saharan Africa and India.
The primary efficacy outcome was “unfavorable status” — defined as “treatment failure or change, loss to follow-up during treatment, TB recurrence, or death” — by 72 weeks.
Results: The percentage of children with an unfavorable status by week 72 did not differ significantly between the two groups, thus achieving the hoped-for result – “noninferiority” (i.e., efficacy) of the abbreviated regimen.
4. Endovascular Therapy for Acute Stroke with a Large Ischemic Region
The study aimed to compare medical care plus endovascular therapy – removal (by several possible interventions) of the clot that had caused a large ischemic stroke – with medical care alone.
The primary outcome was a measure of disability at 90 days. Secondary outcomes included a shift toward a better outcome at 90 days and an improvement of at least 8 points in the National Institutes of Health Stroke Scale (NIHSS) score (range, 0 to 42, with higher scores indicating greater deficit) at 48 hours.
Results: The study found that “among patients with acute stroke and a large ischemic region, functional outcomes at 90 days were better with endovascular therapy and medical care than with medical care alone, but endovascular therapy was associated with an increased incidence of intracranial hemorrhage.” However, “the difference in the percentage of patients with symptomatic intracranial hemorrhage was not significant.”
This NEJM article described a Phase 2-3 double-blind, randomized, controlled trial in which symptomatic, unvaccinated, non-hospitalized adults at high risk for progression to severe Covid-19 were assigned to receive either Paxlovid (which contains the antiviral nirmatrelvir plus ritonavir, which keeps the blood levels of nirmatrelvir elevated) or placebo every 12 hours for five days. The endpoints were viral load and Covid-19–related hospitalization or death from any cause through day 28.
Results: The results were stunning: “Treatment of symptomatic Covid-19 with nirmatrelvir plus ritonavir resulted in a risk of progression to severe Covid-19 that was 89% lower than the risk with placebo, without evident safety concerns.”
It turned out that despite that observation about safety concerns in the trial, the presence of ritonavir causes potentially harmful drug-drug interactions with many commonly prescribed drugs, but the clinical trial reported in the NEJM was, nevertheless, a game-changer. Paxlovid has been the mainstay of treatment for Covid-19 for the past year.
6. Calorie Restriction with or without Time-Restricted Eating in Weight Loss
A reduction in the intake of calories is a primary weight-loss strategy for obese persons, but most diet trials have shown only modest weight loss after a year, and maintaining weight loss is challenging. Time-restricted eating has been proposed as an alternative. It is focused on meal timing instead of caloric intake and requires eating only during specific hours and fasting at all other times.
The NEJM article reported the results of a randomized trial of time-restricted eating plus daily calorie restriction compared to daily calorie restriction alone in obese patients.
Results: “Among patients with obesity, daily calorie restriction with a regimen of time-restricted eating offered no weight-loss benefit as compared with daily calorie restriction alone.”
7. Two Phase 3 Trials of Baricitinib for Alopecia Areata
Alopecia areata is an autoimmune disorder that causes rapid, nonscarring hair loss and, often, stress and anxiety to patients suffering from it. The NEJM article reported the results of two multinational, randomized, placebo-controlled, phase 3 trials (BRAVE-AA1 and BRAVE-AA2) of treatment with baricitinib, an oral, selective, reversible inhibitor of Janus kinases (JAKs) 1 and 2 on hair regrowth in adults with severe alopecia areata.
Results: The results were promising. After 36 weeks, 39% of the patients in BRAVE-AA1 and 36% of those in BRAVE-AA2 who received baricitinib at 4 mg daily had at least 80% scalp coverage with hair. In the two trials, there was complete or near-complete hair regrowth in 23% of patients.
8. PD-1 Blockade in Mismatch Repair–Deficient, Locally Advanced Rectal Cancer
Standard treatment for locally advanced rectal cancer -- neoadjuvant chemotherapy and radiation, followed by surgical resection of the rectum -- is associated with substantial complications and side effects. The article in the NEJM reported a prospective, phase 2, single-group study of the efficacy and safety of neoadjuvant therapy with the programmed death 1 (PD-1) inhibitor dostarlimab in patients with mismatch repair–deficient stage II or III rectal adenocarcinoma. (The rationale, according to the authors: "A subset of rectal
cancer is caused by a deficiency in mismatch repair. Because mismatch repair–defi-
cient colorectal cancer is responsive to programmed death 1 (PD-1) blockade in the
context of metastatic disease, it was hypothesized that checkpoint blockade could be
effective in patients with mismatch repair–deficient, locally advanced rectal cancer.")
A key primary endpoint was the overall response to dostarlimab alone or to dostarlimab plus chemoradiotherapy.
The results were stunning. 12 of 16 enrolled patients had completed six months of dostarlimab therapy at the time the article was written. All had a complete clinical response, with no evidence of tumor on any diagnostic test. During a median follow-up of 12 months, no patient received chemoradiotherapy or underwent surgery, and none had disease progression or recurrence.” No severe adverse events were recorded.
9. Tirzepatide (Mounjaro) Once Weekly for the Treatment of Obesity
The article in the NEJM reported the results of an international, Phase 3, double-blind, randomized, placebo-controlled trial of tirzepatide in non-diabetic adults who were obese or overweight. Tirzepatide is a dual glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist already approved by the FDA to treat Type 2 diabetes.
Results: Both the percentage change in weight and the percentage of participants with at least 5% weight reduction were significantly greater with all three doses of tirzepatide than with placebo. Gastrointestinal adverse events, including nausea, diarrhea, and constipation, were the most common ones reported, but most were transient and only mild to moderate in severity.
10. Multicenter, Randomized Trial of a Bionic Pancreas in Type 1 Diabetes
The holy grail of insulin administration to Type 1 diabetics has long been an indwelling, bionic, fully automated “artificial pancreas” that could make all dosage decisions and deliver insulin autonomously, without carbohydrate counting or other patient inputs.
This NEJM article reported a multicenter, parallel-group, unblinded, randomized trial to test the efficacy and safety of a bionic pancreas compared to standard care in children and adults with type 1 diabetes. Subjects were assigned either to automated glucose control with the bionic pancreas (with insulin aspart or insulin lispro) or to standard care with their current insulin-delivery method (multiple injections, pump, or hybrid closed-loop system) plus a continuous glucose monitor. The primary outcome was the glycated hemoglobin level at 13 weeks.
Results: “In children and adults with type 1 diabetes, use of a bionic pancreas for 13 weeks resulted in a greater reduction in the glycated hemoglobin level than standard care, with no apparent safety concerns.”
Comment: Extensive use of the bionic pancreas could constitute a significant advance for Type 1 diabetics concerning glycemic control, lifestyle, and reduction of disease complications.
11. Treatment for Mild Chronic Hypertension during Pregnancy
The NEJM article reported an open-label, multicenter, randomized trial in which pregnant women with mild chronic hypertension and single fetuses at a gestational age of less than 23 weeks received antihypertensive medications recommended for use in pregnancy compared to a control group that received no such treatment unless severe hypertension (systolic pressure, ≥160 mm Hg; or diastolic pressure, ≥105 mm Hg) developed. The primary outcome was neonatal death or a composite of pregnancy complications.
Results: In pregnant women with mild chronic hypertension, targeting a blood pressure of less than 140/90 mm Hg was associated with better pregnancy outcomes than reserving treatment only for severe hypertension.
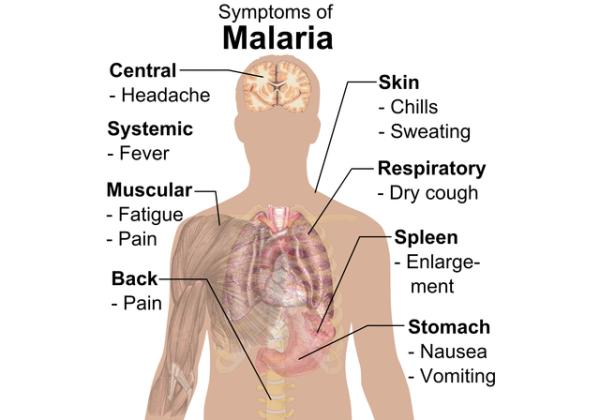
12. Safety and Efficacy of a Monoclonal Antibody against Malaria in Mali
The NEJM article reported a double-blind, randomized, placebo-controlled Phase 2 trial of the monoclonal antibody CIS43LS to prevent infection by P. falciparum (the parasite that causes malaria) in healthy adults over a 6-month malaria season in Mali.
330 adults were assigned to receive a single intravenous infusion of CIS43LS (10 mg per kilogram of body weight or 40 mg per kilogram) or placebo. The primary efficacy endpoint was preventing P. falciparum infection through week 24.
Results: P. falciparum infections were detected on blood-smear examination. At six months, the efficacy of 40 mg of CIS43LS per kilogram compared to placebo was 88.2%, and the effectiveness of 10 mg of CIS43LS per kilogram compared to placebo was 75.0%. Moderate headache with the higher dose of CIS43LS was the most prominent side effect.
Comment: The administration of this safe and effective monoclonal antibody drug could be a game-changer for both public health and economic growth in countries where malaria is endemic.
The NEJM’s “Notable Articles” of 2022 offer an interesting, albeit limited, snapshot of medical progress. As in medical research generally, most are incremental advances, with a few very welcome breakthroughs.