If you want to protect yourself from COVID-19 and have to commute by train as so many do in the tri-state area of New York, New Jersey, and Connecticut, where is the best place to sit socially distant? A new study from China offers some considerations.
The authors begin by acknowledging that train transportation is a common form of mass transit and then make use of one of China’s acknowledge “strengths,” its surveillance system, to track and trace train passengers. In the two-week run-up to China’s New Year and just before the locking down prompted by Wuhan, 150 million Chinese took high-speed rail. For their study, the researchers made use of 2,568 confirmed cases of COVID-19 who had ridden the rails between mid-December and early March. They identified an additional 72,000 close contacts, e.g., individual sitting within three rows of a positive case in the fourteen days incubation period, proceeding the onset of symptoms. With knowledge of the index patient’s seat, as well as their destinations, they could calculate both the spatial and temporal spread of the disease.
- Despite a large number of contacts, only 234 new cases were identified and labeled as coming from a train borne contact. The term attack rate expresses the ratio of new cases to the overall population, in this case, 234/72,000 or an attack rate of 0.37%
- While the attack rate in the row did vary, lowest by the window, highest in the middle, and intermediate in the aisle, none of the differences were statistically significant.
- The individuals in the same row were at the highest risk. Individuals in the two rows behind the index patient had a tenth of the risk of those in the index row. Individuals in the third row back were half again the risk of those rows.
- The individual next to the index patient, carried the highest risk, no surprise there. And that risk rapidly dissipated plateauing at the 4th seat over (the researcher’s termed that the 4th column)
- The average attack rate increased for every hour of co-travel. Again, the further one was away from the index case, either by row or column, reduced the effect of travel time. Those in different rows had less effect of travel time than those in different seats of the index row.
- A passenger sitting in a seat previously occupied by the index patient had a slightly higher increase risk. Still, it was no different than the aggregate for anyone within three rows or six seats of the index case – there was no heighten risk for taking the “contaminated” seat.
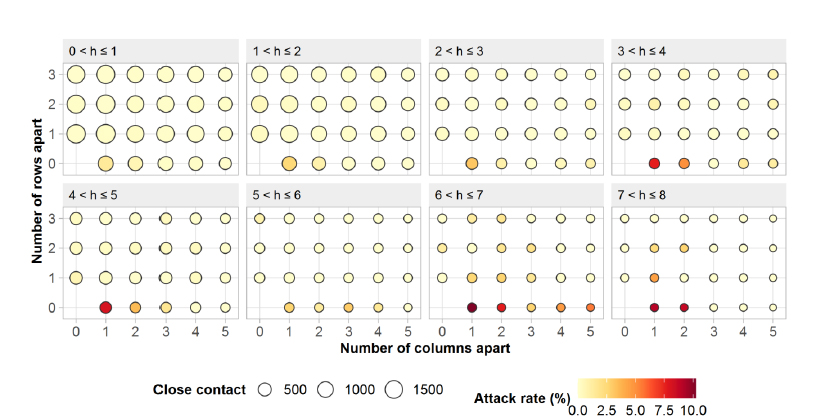
Image Credit University of South Hampton
As with all things COVID, the findings vary; it is of greater risk being in the same row with an index patient, but this might reflect the fact that these people are traveling together and share much more than train time. It might also be due to ups and downs on getting something to eat or going to the bathroom on longer trips. The risk drops off as the distance, measured by rows, increases, and the authors speculate that this may be due to the physical barriers that headrests create.
What the researchers add to our discussion is the temporal component. As the time of the co-travel increased, so did the necessary, safe social distancing. They recommended spacing of two empty seats, not one, in travel over 3 hours. While the work supports social distancing, it suggests that the “safest” social distance within confined spaces may expand over time and should be considered in the allotting of seats. This should not be surprising as the “dose” of COVID we receive is related not only to our social distance but how long we remain in proximity. Track and trace considers 15 minutes or more within a meter to be a close contact.
The study, of course, has limitations, with respect to passenger movement on the train, as well as to their co-travel once they disembarked. It does not take into account the use of masks or face shields, nor does it consider the impact of the ventilation systems.
Source: The risk of COVID-19 transmission in train passengers: an epidemiological and modeling study Clinical Infectious Disease DOI: 10.1093/cid/ciaa1057




