
With rising rates of childhood obesity, the American Academy of Pediatricians has revised its treatment guidelines – pushing for more aggressive management than their previous watchful waiting. Within a short time, the guidelines were assailed as standing on “shaky ground.” STAT captures the entire controversy here. It is a controversy replete with all the usual concerns, unintended consequences, misleading citations, and unwarranted conflicts of interest. If there was a Big Distrust of Science playbook, the concerns hit all the notes.
As a contributor to the Internet of “word bites,” we could expand and amplify STAT's concerns so clearly chronicled, but that is not how science works. I suggest that if we look upstream at our consensus on the issue of obesity, we might see the root of the problem. I turn to the Diagnostic Studies Manual, the psychiatric diagnostic Bible, to understand the current scientific consensus.
“Finally, as was the case in DSM-IV, obesity is not included in DSM-5 as a mental disorder. Obesity results from the long-term excess of energy (calorie) intake relative to energy expenditure. Genetic, physiological, behavioral, and environmental factors that vary across individuals contribute to the development of obesity; thus, obesity per se is not considered a mental disorder.”
The five recognized eating disorders are anorexia nervosa, bulimia nervosa, binge-eating disorder, avoidant-restrictive food intake, and other specific feeding or eating disorders. You can find their diagnostic criteria as identified by the AAP here. In each instance, there is a behavior underlying the diagnosis, but for obesity, one’s weight is pathognomonic, which is a medical term for solely diagnostic.
On the other hand, here is the AAP’s diagnostic criteria for obesity.
“Overweight and obesity: Overweight is defined as a BMI at or above the 85th percentile and below the 95th percentile for children and teens of the same age and sex. Obesity is defined as a BMI at or above the 95th percentile for children and teens of the same age and sex.”
It is not a behavior at all; it is a weight class.
“Obesity is a medical condition characterized by the accumulation of excess body fat. It is typically the result of an imbalance between calorie intake and energy expenditure.”
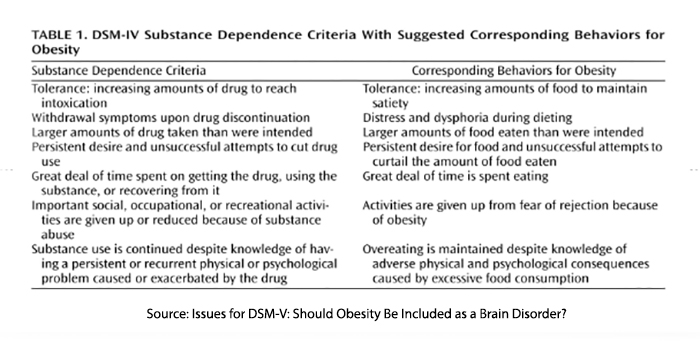
There was controversy in rejecting obesity as a mental disorder in the DSM, but here is one salient argument – that some instances of obesity may be a food addiction.
Would that add to the stigmatization of the obese?
Some would argue that it is impossible to be addicted to food because we need food to survive, whereas there is no evidence that we require nicotine, cocaine, or alcohol. Others describe how Big Food is addicting us to ultra-processed foods designed to trigger pleasure.
One of the prime movers in the AAP’s re-evaluation was the advent of highly effective treatments for obesity, including surgical intervention and the GLP-1s. Watchful waiting was no longer the best option for many. Interestingly, the impact of GLP-1s in lessening the grip of two well-characterized addictions, alcohol and drugs of abuse, suggests that perhaps we might reconsider our definition of obesity – if not in every instance, that possibly many.
Does any of this definitional navel gazing matter?
It can be that, ultimately these definitions guide policy, just as AAP is trying controversially to do. If obesity is not a food addiction, then why must we concern ourselves with the addictive nature of some foods? Wouldn’t our free will keep us from straying off the nutritional high road? If it is an addiction or a behavioral difference, then doesn’t it deserve to be on the spectrum of eating disorders where we can direct research and treatment? Or maybe obesity is a bit of both, making it once again more complex than social media would like us to believe.



