
Clinical background
Orthopedic surgeons are probably the most protocol-driven group I have worked with. While they care for a range of emergencies, their physician extenders, physician assistants, or nurse practitioners can address many of the simpler fractures and sprains. Most hip fractures, on the other hand, demand urgent surgical intervention. Because these occur primarily in the elderly with other co-morbidities, orthopedists, having foresworn any medical thought outside orthopedics, generally have hospitalists or other internal medicine types “optimize” these patients before taking them to the OR within 24 hours. This allows for safer surgical care and outcomes and lets the orthopedist sleep through the night and face those urgent cases as a part of their workday.
The study at hand comes from the UK, where waiting for healthcare is increasingly disgraceful. In addition to long waits for elective care, waits in the Emergency Department (ED) for any reason can be equally interminable.
“The 4-hour wait standard in the ED was established in England in 2004 … under this standard, most patients arriving at the ED must be admitted or discharged within 4 hours. Although this standard was not based on evidence, there has been a growing body of evidence that failure to achieve this timeframe is associated with increased patient mortality.” [emphasis added]
With that standard in mind, the current study, part of a quality improvement program, looked at the outcomes of patients undergoing operative care for a hip fracture with specific regard to the amount of time spent in the ED. The study involved a single trauma center serving a 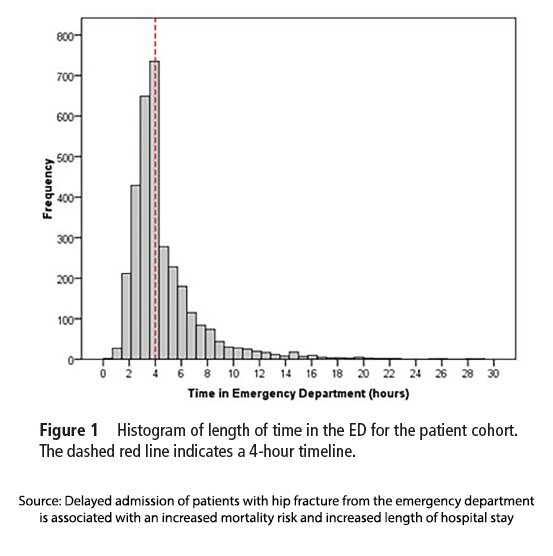 population of about 1 million in Scotland over a 3½ year interval – during which there were 3,266 surgically repaired hip fractures. The average age was 81, the patients predominantly female, and the “median time to theatre from admission to the ward was 22.5 hours.” (I so love the use of theater over operating room.)
population of about 1 million in Scotland over a 3½ year interval – during which there were 3,266 surgically repaired hip fractures. The average age was 81, the patients predominantly female, and the “median time to theatre from admission to the ward was 22.5 hours.” (I so love the use of theater over operating room.)
- Patients were considered “delayed” if their time in the ED before admission exceeded four hours. The graph shows how good physicians are at meeting goals; we are truly a group that trains for the test.
- Over one-third (38.6%) of the patient cohort experienced a 4+ hour delay in being admitted from the ED.
- Those experiencing delays were more likely to be admitted in the winter and have higher risk scores as measured by ASA [1]
- Those patients had a one-day longer hospital stay.
- Patients who experienced delays had a significantly lower survival rate at 60 and 90 days after their injury and at the final follow-up, point compared to those who were admitted to the ward within four hours of arriving at the ED.
- The study found an association between increased time spent in the ED and an increased risk of death 90 days after the injury and at the final follow-up point, even when controlling for other potential contributing factors. This meant for every 36 patients who experienced delays, there was one additional death (estimated 35).
The researcher’s statistical analysis led them to conclude,
“This study has demonstrated that in patients with a hip fracture at our trauma centre, staying longer than 4 hours in the ED was independently associated with a significantly greater mortality risk at 60 and 90 days and at final follow-up.”
Of course, statistics cannot untangle the interdependence of time in the ED with other factors. When considering each factor independently, ED delay indeed resulted in a 36% increase in 90-day mortality, but
- Higher ASA score accounted for a 115% increase
- Admission from a long-term care facility, where we can safely assume patients have more life-impacting illnesses, increased mortality by 129%
- More complicated fractures increased mortality by 1100%.
I would argue that the additional time in the ED was a temporal marker of significant co-morbidities rather than a genuinely independent risk factor. The researchers admit to that near the end of their article, writing,
“The major limitation is that we did not adjust for patient acuity and factors delaying their admission, such as being medically unwell, which may be influencing their outcome.”
An interesting aside for those who may wonder why winter admission results in greater mortality is that winter has been shown to have an increased prevalence of respiratory infections, which can also lead to pre- and post-operative concerns.
Much like the proverbial drunk searching under the street lamp for his lost keys, the researchers focused on what they could measure, time in the ED, rather than the more complex, unquantifiable factors like patient acuity or underlying health conditions that may have influenced these delays. As the researchers admitted, they didn’t adjust for the severity of the patient’s medical issues, leaving us to question whether the extra time in the ED was the culprit or simply a marker for more significant health problems. Ultimately, while this study highlights a pressing need for improved efficiency in emergency care, it also reminds us that not all risks are quickly captured by statistics. It also demonstrates the advocacy role scientific publications can take in improving the abysmal time delays associated with healthcare in the UK.
[1] American Society of Anesthesiologists (ASA) grading system is routinely used pre-operatively to judge operative risk. In this instance, more patients delayed in the ED had a score of 4, “A patient with severe systemic disease that is a constant threat to life,” vs. a score of 3, “A patient with severe systemic disease.”
Source: Delayed admission of patients with hip fracture from the emergency department is associated with an increased mortality risk and increased length of hospital stay BMJ DOI: 10.1136/ emermed-2023-213085



