Proper functioning of the human body relies on microbial partners. The sum total of these partners, called the microbiome, plays a myriad of important roles in maintaining human health -- from facilitating digestion to developing the immune response.
Each person's microbiome may be unique. However, research has linked certain microbial compositions to good health and other compositions to bad health. This shift in the contents of the microbiome, known as dysbiosis, has been linked to a variety of disease states, such as periodontitis (gum disease), otitis media (middle ear infection), obesity, and inflammatory bowel disease. In a new review article, a team of scientists explores the link between the microbiome and cirrhosis.
Cirrhosis is the final stage of liver disease, which can be brought on by hepatitis, excessive alcohol consumption, or excess fat storage in liver cells. When the liver is damaged and then repaired, scar tissue is left behind. Unfortunately, scarred tissue is nonfunctional, so cirrhosis leads to death. In fact, cirrhosis is the #12 most common cause of death in the U.S.
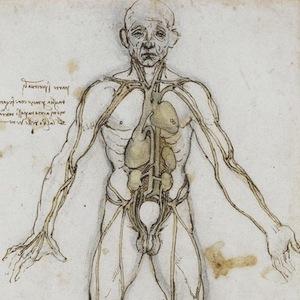
Regardless of the immediate cause of liver disease (e.g., booze or viral hepatitis), the underlying problem in all cases is likely to be inflammation. Inflammation damages the liver, resulting in scarring. The authors believe that dysbiosis in the gut and oral cavity -- that is, an unhealthy composition of the microbiome in those body parts -- may exacerbate this condition. (See image.)

The bacteria in our intestines are supposed to be confined to that organ. However, alcohol, dysbiosis, or other conditions can cause the intestinal barrier to become "leaky," allowing bacteria or their inflammation-inducing molecules to cross into the bloodstream*. Similarly, in addition to being linked to periodontitis, oral dysbiosis has been associated with diabetes, cardiovascular disease, and liver disease. Therefore, it is quite possible that unhealthy bacteria in both the mouth and gut can cause inflammation throughout the entire body, aggravating conditions like cirrhosis.
As a result, the authors suggest the existence of an oral-gut-liver axis for cirrhosis -- a microbial axis of evil, if you will. Of course, it is possible that dysbiosis is a result rather than a cause of liver disease. Perhaps even more likely is that what scientists are witnessing is a negative feedback loop; that is, liver disease causes dysbiosis, and dysbiosis worsens liver disease.
If their model is correct, what can be done about it? Judicious use of antibiotics and probiotics to reverse dysbiosis or lessen its impact would be one possibility. The best advice, though, is to avoid liver disease in the first place. That means drinking in moderation, receiving a hepatitis B vaccine, avoiding contracting hepatitis C (e.g., by having unprotected sex or sharing needles), and maintaining a healthy weight.
Note: "Leaky gut syndrome" is not a real medical diagnosis.
Source: Chathur Acharya, Sinem Esra Sahingur, and Jasmohan S. Bajaj. "Microbiota, cirrhosis, and the emerging oral-gut-liver axis." JCI Insight 2 (19): e94416. Published: 5-Oct-2017. doi: 10.1172/jci.insight.94416.