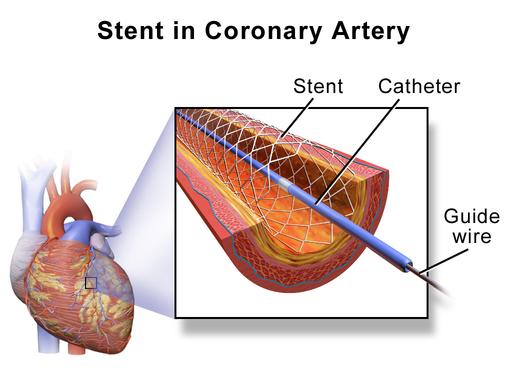
The world of interventional cardiology was rocked last week with a study showing that stenting, placing a tiny metal scaffold to open up a single coronary artery to relieve chest pain (angina) was no better than optimal medical management. Angina is a sign that the heart is not getting enough blood and that there is danger of a heart attack or myocardial infarction (MI), when part of the heart muscle dies reducing the heart’s ability to pump blood. A bad thing. My colleague, Julianna LeMieux, covered the study last week. Today, I want to talk about an essential feature of the study’s control group, those participants who volunteered for sham surgery. Sham surgery in this instance is identical in every way to the stenting with one exception; there was no therapeutic intervention, no stent was placed.
Fewer and fewer studies of medications or procedures use placebo control, they are mostly non-inferiority studies showing that the medication or procedure is at least as good as the current standard. But when the control group doesn’t include a placebo how can we tell that the intervention has any efficacy; after all the placebo-effect can be as much as 33% of the response. There is a certain irony in that the first popularized study in which a sham surgical procedure was performed regarding the question of angina; evaluating the effect of tying off the internal mammary artery (IMA). This artery runs along the inside of the chest providing blood to our breastbone and ribs. Medical science, in 1959 already knew that angina was due to the heart being deprived of oxygen and that in an attempt to increase blood flow, the coronary circulation developed small accessory or collateral pathways. It was thought that the IMA which is a larger vessel competed with these small collaterals and ‘stole’ blood from the heart. So some physicians felt that by tying off the IMA it would decrease the competition and result in more blood flow, more oxygen and less angina. And they had case reports that showed tying off the artery resulted in less angina in their patients. Better yet, the had a study of 304 patients, all who underwent IMA ligation and 57% experience excellent or good improvement in their symptoms within a month! And those good effects lasted for 90% of them for many months or years.
The study that refuted this finding, by using a sham surgical procedure was published in 1959. I hasten to add that by today’s standards it would not be accepted for publication. Underpowered, with only seventeen patients in total; the demographics not quantified although all the patients had “seriously limited by angina;” and serious concerns about randomization since all of the five women in the study were in the ligation group. They concluded
“From the results in this rather small group of patients, bilateral skin incisions in the second intercostal space seems to be at least as effective as internal mammary artery ligation in the therapy of angina pectoris.”
And while the subsequent firestorm was not as great as with the current study of stenting, there were questions raised about the ethics of such a sham surgery placebo control. Again in the words of the authors
“A reasonably optimistic attitude on the physicians’ part was maintained. The subjects were informed of the fact that this procedure had not been proved to be of value and yet many were aware of the enthusiastic report published in the Reader’s Digest. The patients were told only that they were participating in an evaluation of this operation; they were not informed of the double-blind nature of the study.”
Coming just fifteen years after World War II, some felt that this type of research violated the Nuremberg Code which required that all research avoid “any unnecessary physical or mental suffering, and the degree of risk to be taken should never exceed the humanitarian importance of the problem to be solved by the experiment.” Sham surgery without any benefit and even with a small risk, as evidenced by the current stenting study, was felt to violate minimizing harm. Others, more economically inclined, saw the potential savings to society from unnecessary surgical care tipping the balance of risk versus benefit away from risk.
I have written about surgery’s placebo effect here. That meta-analysis of sham surgery as the control group found half of the studies reporting adverse events. But only a small fraction was in the control arm, in many cases, the incidence of adverse events in the control arm was less than 5%, consistent with the current study where four control patients required further invasive intervention. Is a 5% complication rate in the placebo arm worth the risk? What if there had been a death?
Let me share what cardiologists have known for a long time, dilating a coronary artery with a balloon or placing a stent to enlarge the opening within the artery, in patients with stable angina, does not reduce the deaths from heart disease or the number of subsequent heart attacks. It is done only to improve symptoms and the quality of life. Surprise!
The disagreements about the stenting study and chest pain center on the small size of the study making it underpowered; the short follow-up period of six weeks making it difficult to talk about a more chronic response; and of course, the fact that in medically optimizing the patients before any randomization, physicians spoke and check on them three times a week, definitely not a real-world level of care. Other physicians argue that the findings will be inappropriately generalized to different patient populations.
In a world of me-too studies, this work is to be commended. It has demonstrated that placebo/sham controls are both possible and useful. It has shown once again for those of us who intervene how strong the placebo response can be. The study has limitations; I will let the cardiologists discuss the nuanced flaws, But the research suggests that we need to reconsider how procedures find their way into accepted practice and it also demonstrates a way forward.
[1] To our younger readers, Reader’s Digest was the media version of Facebook a generation ago, there are no national media with its reach today, including the pale version of Reader’s Digest still available.