Anthem is back in the news. You might remember that just a short while ago Anthem refused to pay for Emergency Department care they deemed not to be an emergency. [1] Their latest attempt to rein in their costs is restricting access to anesthesiologists or nurse anesthetists for many cases of cataract surgery.
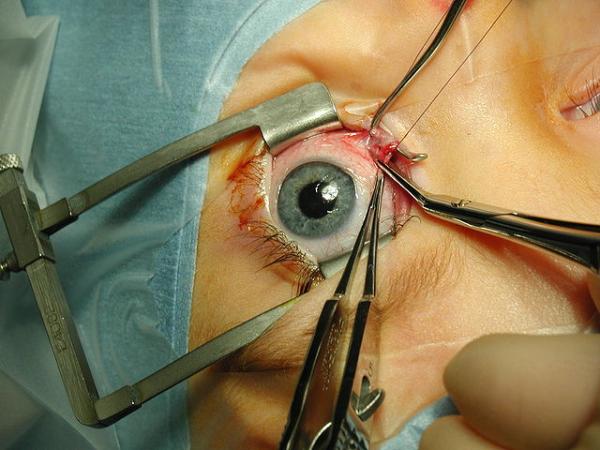
Cataract surgery involves cutting the lens of the eye, removing the deposits creating a cloudy vision and replacing the lens. It is a very common procedure, especially in the Medicare population. The eye can be anesthetized, so that the patient does not feel pain, with topical medications. But patients have to lie still. Some patients are physically not capable of lying flat, some patients are just too anxious about someone cutting their eye, and they need a bit of sedation, the medical term is conscious sedation. Patient’s getting conscious sedation are usually given medications in their veins to sleep for a short while during the procedure. Anthem’s new guidelines have no problem with the use of conscious sedation; their concern is that many physicians have that part of the care provided by an anesthesiologist or nurse anesthetist, which costs them more money.
When an anesthesiologist or nurse anesthetist provides conscious sedation, it is called monitored anesthesia care or MAC - the care that Anthem’s new guidelines want to end unless certain preconditions are met. Specifically MAC can be approved for patients under age 18, and those patients unable to cooperate or communicate because of medical conditions. There are also exemptions for those who have failed this approach or where surgery is anticipated to be prolonged or complex. But what about the rest of the patients, the bulk of the patients undergoing cataract surgery?
Anthem understands the role of these providers; they are actually delineated in their guidelines. Their care includes:
- Diagnosis and treatment of clinical problems that occur during the procedure
- Support of vital functions
- Administration of sedatives, analgesics, hypnotics, anesthetic agents or other medications as necessary for patient safety
- Psychological support and physical comfort
- Provision of other medical services as needed to complete the procedure safely
They are not there to push drugs; they are there to protect the patient during a procedure. Anthem judges that this additional protection is unnecessary or at least that it can be provided in the same way by the operating surgeon.
As a surgeon, I have a love-hate relationship with anesthesiologists. They make the case longer; they cancel cases when they feel we could improve the patient’s preoperative preparation. But when things go sideways during surgery, they have been there to keep that patient alive and let me do what I do best, operate. They are crucial members of the operating room team. Let me frame this in another way, provision of monitored anesthesia care prevents distracted surgery.
In the latter part of my career, I spent more time in the catheterization laboratory doing endovascular procedures, than in the operating room cutting people open. The catheterization laboratory is a different creature from the operating room; cardiologists often administer conscious sedation without an anesthesiologist present – they feel comfortable providing anesthesia while doing the procedure. As a surgeon, raised in operating rooms where an anesthesiologist was required I was uncomfortable because I could not meaningfully attend to my surgery and the patient's vital signs, comfort and safety simultaneously. It is no different than say, texting while driving, and we already know how well that goes.
Here is Anthem’s conclusion:
“…there is no one definitive approach to anesthesia for cataract surgery. The use of anesthesia during procedures should be balanced with the potential risk of harm to those individuals who are sedated during pain procedures. … It is a guideline for when MAC and general anesthesia, which require the service of an anesthesiologist, CRNA, or other certified personnel is appropriate and medically necessary …”
It is not up to any insurance company to determine what is the safest way to care for a patient, not as long as I and our legal system hold myself accountable for those judgments. This decision supports distracted care. There are other ways to reduce costs besides jeopardizing patients.
[1] The patient chose to seek care in the Emergency Department rather than from a practitioner or urgent care center. After the care was provided, with the advantage of hindsight Anthem determined whether the care was provided in “an appropriate setting.” When they deemed it inappropriate, the patient and Emergency Department were left with the charges. Patients are not good at knowing what an emergency is, that is why they are patients and not doctors.