I live on the East End, that part of Long Island where the island forks into its north, agriculture, and fishing, and it’s south, more associated with the Hamptons, summer home for the beautiful people; but it was not always so. Once the Hamptons were about fishing and agriculture too, in fact, many of its settlers were fleeing south from Salem, Massachusetts in the years we associate with Cotton Mather and the witch trials. Those Hampton’s channeled a Cape Cod vibe,
“…a drowsy, secluded village at the extreme end of Long Island; settled by New Englanders, it has the attractive characteristics of their villages-the long common green, the beautiful well-kept trees, and the comfortable, substantial houses, each with an individual air combined of self-respecting, secluded dignity and kindly hospitality”
There is something to the beautiful juxtaposition of scrub pine forests and beaches with long vistas of sea and sky.
“Driving with my father through a wooded road leading from East Hampton to Amagansett, we suddenly came upon two women, mother and daughter, both bowing, twisting, grimacing. I stared in wonderment, almost in fear. What could it mean? My father paused to speak with them, and we passed on.”
Huntington’s Disease
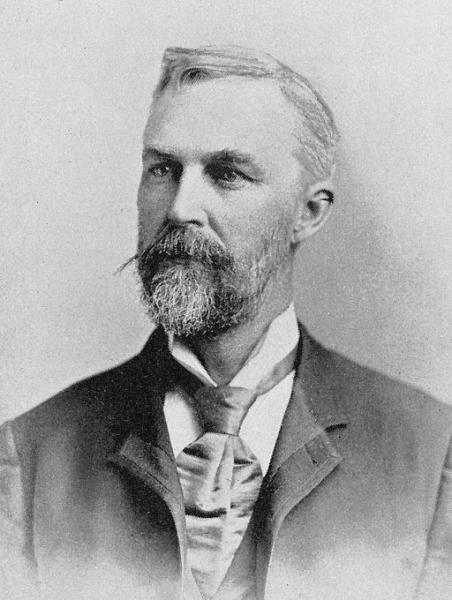
The author of those words, George Huntington, the physician credited with defining the disease that carries his name, Huntington’s Disease, a genetic, invariably fatal, neurologic disorder. Those twisting, grimacing alterations in body movement are called chorea and begin with small unintentional movements, perhaps a momentary lack of coordination but over time become more dominant, resulting in increasing inability to navigate the environment and eat. Those physical manifestations are accompanied by increasing dementia and the mental disabilities of depression, anxiety, compulsive behavior, and suicide.
“The hereditary chorea, as I shall call it, is confined to certain and fortunately a few families, and has been transmitted to them, an heirloom from generations away back in the dim past. It is spoken of by those in whose veins the seeds of the disease are known to exist, with a kind of horror, and not at all alluded to except through dire necessity, when it is mentioned as “that disorder.”… When either or both the parents have shown manifestations of the disease, … one or more of the offspring almost invariably suffer from the disease, if they live to adult age. But if by any chance these children go through life without it, the thread is broken, and the grandchildren and great-grandchildren of the original shakers may rest assured that they are free from the disease. …Unstable and whimsical as the disease may be in other respects, in this it is firm, it never skips a generation to again manifest itself in another; once having yielded its claims, it never regains them.” George Huntington
The Huntington gene is found throughout our bodies, it’s exact role unclear. Part of the gene contains a repeating section of nucleotides, CAG, which vary in length. In individuals unaffected by Huntington’s, the repeat occurs less than twenty-six times. As the repeat increases, the replication of the gene becomes increasingly less stable, creating genes with more and more of the repeats. These repeats cause the protein produced by the gene, Huntingtin, to enfold in an abnormal configuration resulting in cumulative neurologic injury. Similar to the action of the abnormal proteins identified in Alzheimer’s Disease. While it is genetically dominant, that is, it can be inherited from either parent, there is a spectrum of presentation. As the repeats increase, an individual is more likely to experience the symptoms of Huntington’s Disease. Those individuals with 36 to 39 repeats may or not be affected, while those with 40 or more repeats will become victims. Unlike other genetic diseases, which present more frequently in infants or children, the age of onset for Huntington’s is in the 30’s, long after many individuals have become parents and passed the genetic risk to their children.
Medicine has yet to find a cure. Accurate diagnostic testing is only 25 years old, a blood test to characterize the number of repeats in the Huntington gene. In the time before a reliable test was available, many individuals at risk, in the 70-90% range were interested in testing. Once that test became available, the interest plummeted with only a small fraction of at-risk patients, five percent, wanting “to know.” In comparison, the determination of the presence of the BRCA mutation associated with breast cancer, in admittedly small studies, is in the range of 25% or more. What accounts for the differences?
Prospective Huntington At-Risk Observational Study (PHAROS)
“I have never known a recovery or even an amelioration of symptoms in this form of chorea; when once it begins, it clings to the bitter end. No treatment seems to be of any avail, and indeed nowadays its end is so well-known to the sufferer and his friends, that medical advice is seldom sought. It seems at least to be one of the incurables.” George Huntington
Part of the answer may come from a study of participants in this study who choose not to know their Huntington’s Disease (HD) status. The study enrolled asymptomatic patients with a 50% risk of developing HD, the primary goal of the study was to ascertain whether some constellation of early symptoms and signs might alert physicians. The current research, a secondary analysis, focused on the overwhelming number, roughly 87%, that chose not to be tested or know. Their choice was not predicated on access, 60% had no concerns about cost or the vagaries of testing. It had to do with, what I would characterize, but the researchers did not, as a loss of hope. 66% cited a lack of effective treatment or cure and the inability to “undo” the knowledge as their primary motivation. That is clearly one of the differences that we see in BRCA positive women, they may not be able to undo the knowledge, but there are treatments – hope persists.
For many, there was an acceptance of uncertainty, knowing might mean a sure loss of control, in these circumstances, perhaps ignorance is a form of bliss. Slightly more than half anticipated treatment to improve symptoms or postpone the onset of the disease within the next 10 years; more “certain” as to improving symptoms than preventing HD’s onset. Women were more hopeful than men. Asymptomatic patients are more than reluctant to be tested, and that has implications for clinical studies. How can you look for an effective treatment if you have not characterized the patient’s risk; and in characterizing the risk do you not have an ethical obligation to inform the patient?
In January of this year, the FDA approved safety and efficacy trials for a genetic vector that non-selectively reduces Huntingtin, the abnormal protein. [1] Other avenues are also be pursued, including CRISPR, where at least one group has shown an ability to remove those excess CAG repeats. Perhaps the hope expressed by those patients in the PHAROS study is not misplaced. In the meantime, the study should serve as a reminder to us all, physicians and patients, that medicine remains a practical art and that emotions, like hope and fear, sometimes play outsized roles.
[1] The investigational therapy interferes with the messenger RNA (mRNA) that translates the mutated gene into the abnormal protein. A non-infective adeno-associated virus “transports” AMT-130, a small synthetic mRNA binding with the Huntington’ gene’s mRNA targeting it for degradation and lowering the amount of abnormal protein produced.
Sources: The Choice Not to Undergo Genetic Testing for Huntington Disease: Results from the PHAROS Study Clinical Genetics DOI: 10.1111/cge.13529
A biography of George Huntington, MD Bulletin of the Institute of Medicine
The story of George Huntington and his disease
Huntington's Disease and East Hampton