In a poster presentation at the American Academy of Orthopedic Surgery meeting, a paper demonstrates that the cost of hip and knee replacements can be significantly decreased with no change in outcomes and no greater rates of complications. [1] The secret is location, location, location – in this case, a switch from hospital-based to ambulatory care. Here are their findings:
· 252 patients matched for the procedure, age, gender, weight, and health assessment, half undergoing treatment in the hospital, the other half undergoing ambulatory surgery.
· Roughly two-thirds underwent hip replacement; the remaining patients underwent knee replacement
· No “meaningful” difference in complications or readmissions between the groups
· 40% lower cost for patients in an ambulatory care setting, from $19,361 to $11,677. These costs include surgical fees, implants, staffing, medications, and immediate post-operative care. The total length of stay was 23:24 hours for inpatients and 8:09 hours for outpatients
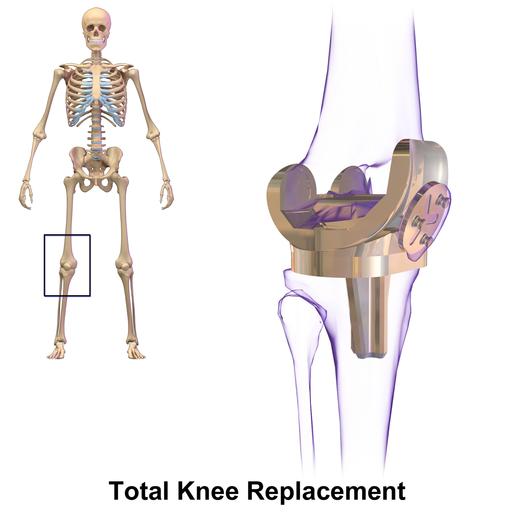
There are several things we can learn from the data. But before raining on the parade let me state how great these results are, the physicians and their teams should be congratulated on their work. It demonstrates the value of standardized care. And one has to be in awe of a health system where people can undergo a major operation, removing and replacing an entire joint in your hip and knee and be safely returned home within a day, let alone 8 hours.
Now, for the rain
The fact that the stays were short indicated these patients are the semi-ambulatory well and may not require as much care to get up and moving. You can call it careful patient selection or cherry-picking. The data on costs is missing and fails to include two essential and overlooked components. First, orthopedists are very careful when it comes to preoperative assessment, so there may be costs for cardiac evaluations and “medical” clearance that adds equally to both ambulatory and hospital care. Second, there is no information on the post-discharge care, and it’s costs, e.g., physical therapy nor do we know whether one group or another required more post-discharge attention or had similar outcomes concerning ambulation. I would suspect that there was no “meaningful difference,” but I don’t know.
Follow the money
Many factors reduce costs in an ambulatory care setting, and we should be mindful of them. First, ambulatory surgery centers (ASC) require less staffing than full-service hospitals, makes sense if for no other reason that you are not open 24 hours a day so that you save on at least one shift. Second, ASCs don’t carry extraneous equipment, like a CT or MRI. These are very focused enterprises, think of them as you might the difference in cost between replacing your muffler at the Midas dealership or in the service department of the car dealership. Those “indirect” costs add up but are part of spreading the cost of running a full-service hospital to everyone.
There is nothing wrong with a highly focused, well-run, ASC but if you remove all the semi-ambulatory well from the hospital, taking the less expensive to care for patients to the ASC, who is left in the hospitals – the sick and not so ambulatory. And as we have seen time and time again, the cost of caring for the sick is greater than that of the well. There is a cost-shifting taking place, and in a sense, we are robbing Peter to pay Paul - and in many cases, Paul is a physician or company who has or feels no obligation to support the hospital.
[1] I do not as a general rule write about reports I have not fully read, and I am basing the factual data on the press release I have reviewed.