
Infections, like all biological phenomena, change and evolve. The poorly-defined Post-Acute Sequelae of COVID (PASC), or “Long COVID,” is no exception. A new study reports on the dynamic incidence of Long COVID over time. To get their findings, the researchers used a healthcare database of veterans maintained by the US Department of Veterans Affairs. They identified roughly 450,000 veterans with a COVID-19 infection over two years. They looked at three COVID-19 variants, pre-delta, delta, and omicron, and separated vaccinated from unvaccinated. (There was no vaccinated group in the pre-delta era because there was no vaccine.) They also identified control groups for each of those intervals of veterans without COVID-19 infection. They followed the patients for a year after their initial infection.
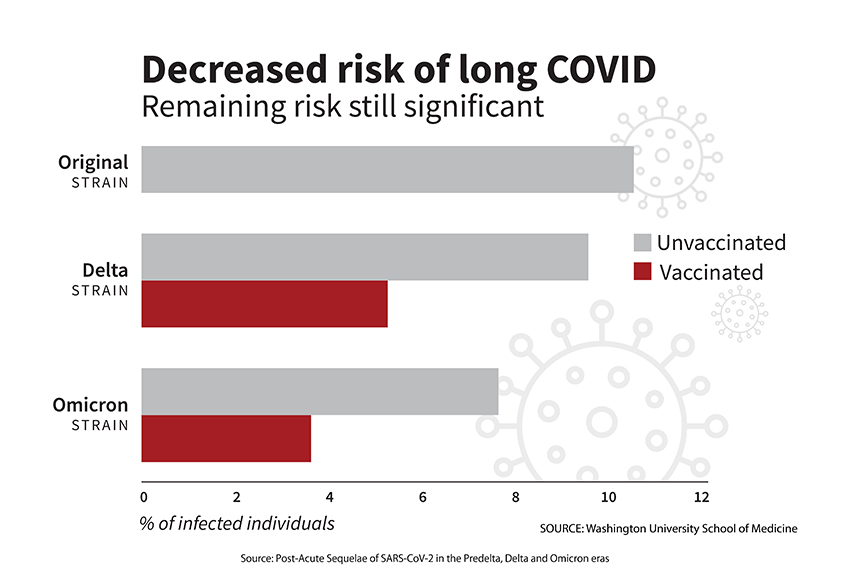
The incidence of PASC was reduced with each successive variant, and the reduction was more pronounced among the vaccinated than the unvaccinated.
They calculated the degree to which PASC resulted in disability, expressed as disability-adjusted life years (DALY). While there was a slight decline in DALY overall, the vaccinated showed the most protection from lost time.
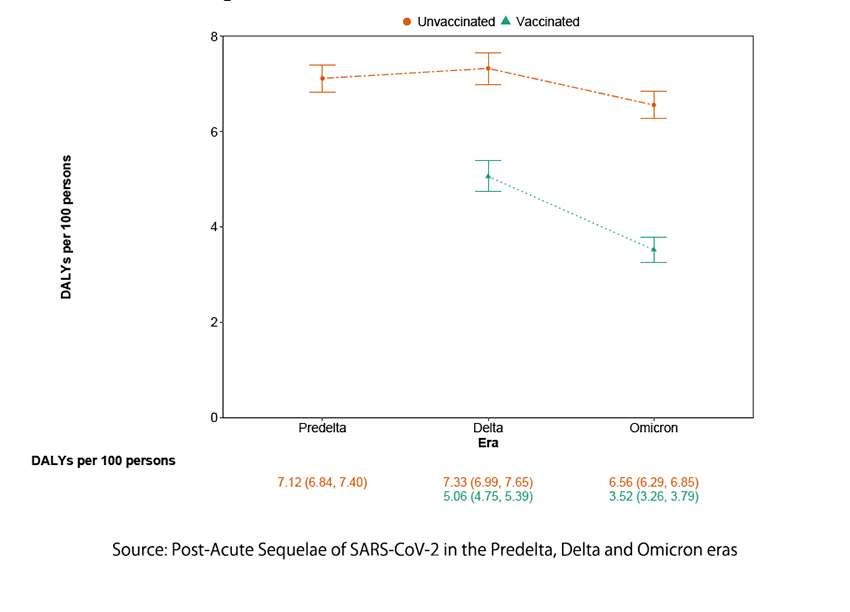
The researchers employed a statistical technique called decomposition analysis to tease out how many of these outcomes were due to the changing virulence of the virus and the effect of vaccination. According to their calculations, the primary driver of the diminishing prevalence of PASC was vaccination, accounting for 70% of the impact, with the remainder being the changing virulence of the virus.
Supporting their belief that the impact of the virus was changing was the finding that the organs impacted by PASC also changed over time. There were more GI and metabolic findings in PASC among the unvaccinated during the omicron era than in other groups, indicating that the incidence and presentation changed. This leads to a simple conclusion:
“In sum, our findings indicate that temporal effects and vaccines have contributed to a substantial decline in burden of PASC…”
As with any study, there are strengths and limitations. The study was of veterans, “older white males,” and there can be undercounting of PASC and COVID infections among the controls. The strengths lie in the database’s comprehensive look at a specific population.
Like chronic fatigue syndrome, PASC remains more of a collection of symptoms - a syndrome - rather than a disease with identifiable biomarkers. However, in this study, the diagnostic criteria for PASC remained constant. The researchers have demonstrated that COVID-19 is a dynamic disease, and the give-and-take between host and infection continues. This is another feature of what we call “herd immunity,” and we mistakenly believe it reflects a static process. One of the lessons of COVID-19 is that we lived through an era where the novel has become, unfortunately, expected. We have done so in the past, but never with as much scientific understanding. That is why, in part, “the science” has changed and why ascribing ill-intent rather than prideful error to our leadership serves no useful function.
Source: Post-Acute Sequelae of SARS-CoV-2 in the Predelta, Delta, and Omicron eras NEJM DOI: 10.1056/NEJMoa2403211



