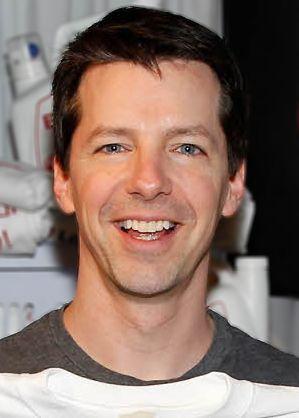
Actor Sean Hayes of television’s Will & Grace fame disclosed on The Ellen DeGeneres Show he experienced a recent health scare. Describing abrupt abdominal pain, he went to the emergency room and was admitted for gastrointestinal (GI) perforation. Laparoscopic surgery was expeditiously performed.
And a couple short weeks later he was able to appear on her show.
In his own words from the television clip, Mr. Hayes recounts his frightening tale with a bit of humor injected:
“I went to bed at night and all of a sudden I felt this excruciating pain in my stomach...So I went to the ER and … thank God I did. I had a very rare thing where my small intestine burst open and it was poisoning my body...They went in there and they clipped off the bad part and put it back together...you know with, like, a chip clip.”
He continues his account and reveals two identical “breathing things” he jokingly refers to as a game from the hospital to “keep your lungs strong” and “don’t get pneumonia or build up fluid.” He challenges Ellen DeGeneres to see who could beat the other in sustaining getting the balls to the top (see video here). These items are called incentive spirometers and are routinely used after surgery, in particular in the postoperative period.
Anesthesia and the accompanying pulmonary assistance provided during surgery warrant its use throughout recovery. Whenever anesthesia is used, there can be a collapse of tiny airways called atelectasis. This (and the anesthesia or narcotics) can put a patient at risk of developing pneumonia as can aspirating. This is why for longer cases, especially, you are encouraged to exercise your lungs by breathing into an incentive spirometer (often hourly) and not immediately be fed a regular meal. Mr. Hayes mentions the use of pain medications. Narcotics, in particular, can slow the respiratory drive causing hypoventilation and depending on the different drugs used altogether a patient might be not alert enough to resume eating quickly-- with a bowel surgery as well there will likely be greater delay imposed too. Knowing all of this is why special care is taken during this time. To learn about important precautions taken with surgery in general, read Bill Paxton Dies of Surgical Complications.
What causes gastrointestinal perforation? Why is it so dangerous?
Perforations can occur anywhere throughout the GI tract, e.g. esophagus, stomach, intestines, colon etc. When there is such a rupture, the contents contained within that purposely confined space get released freely into the abdomen or chest. Bowel contents --albeit stool, bile, stomach acid, food, bacteria or free air-- released into the sterile environment of its surroundings cause tremendous damage, toxicity, incite inflammation and infectious spread. In addition, they can impede neighboring structures. Rapid intervention is often necessary to prevent overwhelming infection (aka sepsis), tissue necrosis, shock and so forth. Conservative measures like bowel rest from not permitting eating or drinking, intravenous fluids or antibiotics are initiated with other supportive efforts.
I discuss the impact of esophageal tears and their life-threatening nature in Screaming At One Direction Concert Not Only Way To Collapse A Lung. In An Article NOT About The Election, I detail how the eating of ghost peppers was the catalyst that triggered Boerhaave Syndrome, a barotrauma-inducing spontaneous esophageal rupture due to extreme retching and vomiting. After consuming ghost peppers in a contest, a 47-year-old man presented to the Emergency Room in severe abdominal and chest pain after violent retching and vomiting. He progressively worsened as his medical work-up revealed a spontaneous 2.5 cm perforation of his distal esophagus with resultant air and food debris in his chest (where air and food should not be) and collapsing of a lung. He was urgently operated on, required multiple chest tubes and remained intubated (aka had a tube down his throat to breathe) for 14 days. He went home on day 23 with a tube in his stomach.
In As Far As Ingesting Foreign Objects Go, Magnets Worse Than Many, I write about a Colorado toddler who required emergency medical intervention after ingesting 28 high-powered buckyball magnets. In this recent case of 2-year-old Ella McBrien, the magnets conjoined in a circular manner that began to erode and obstruct bowel. An early hole was being formed. Thankfully, two attempts with specialized endoscopy solved the problem otherwise these situations can escalate to major surgery involving removal of substantial portions of bowel. Losing segments of bowel can lead to longer term issues.
Where the tear or rupture occurs, depends on the why. This, too, determines the extent of the problem. Among the many causes are:
-
Blunt or penetrating trauma
-
Foreign Bodies--especially sharp ones-- ingested by swallowing from above or inserted from below (see Inanimate Objects in Orifices series). Batteries due to their corrosive nature are particularly dangerous when ingested. As are caustic substances, in general.
-
Iatrogenic causes like complications from surgery, the use of medical scopes (e.g. colonoscopy), biopsies
-
Spontaneous
-
Ulcer disease
-
Cancer
-
Appendicitis
-
Diverticulitis
-
Inflammatory Bowel Disease (e.g. Crohn’s Disease, ulcerative colitis)
-
Medications like long-term use of NSAIDs (non-steroidal anti-inflammatory drugs like ibuprofen, aspirin) or steroids
-
Excessive drinking, smoking increase risks
In the end, the sooner the condition is properly identified and corrected, the better the outcome. When a person is otherwise healthy, they can fare very well under these circumstances. Depending on underlying disease, clinical status or delays in care, complications can be quite extensive and life-threatening.