By Mark Miller, University of Virginia
Twelve patients who tried injections of stem cells were hospitalized with infections, according to a report in The New York Times that should cause patients concern. More important is that they should investigate stem cell treatments, for conditions such as cartilage injuries to their joints, before committing to one of these procedures. It’s also a valuable reminder that physicians need to work closely with patients to help them understand their options and which choice may be best for them.
Stem cells are “uncommitted” cells that are, at least theoretically, capable of becoming any type of cell – skin, heart, kidney or even knee cartilage cells. Stem cells can come from fetal tissue, including products of in-vitro fertilization as well as placenta and umbilical cord tissue. They can also come from a patient’s own “hidden” adult stem cells, which are most often harvested from bone marrow and fat. The potential for using these cells in medicine is tremendous; for instance, stem cell transplants are used frequently to treat certain cancers, such as leukemias and blood disorders.
I am a professor of orthopedic surgery at the University of Virginia. I am also a victim of knee osteoarthritis and have gone through knee replacements for both of my knees a little over a year ago. Since then I have made it my mission to educate the public about this condition, and to try to keep the enthusiasm regarding new cutting-edge options in check. That is because I have seen many patients who have paid thousands of dollars for a so-called stem cell treatment only to discover later that they were duped. In most cases fortunately, the only injury was to their wallet.
According to the Arthritis Foundation, at least 31 million Americans are affected with osteoarthritis, the most common type of cartilage wear. A quick web search will confirm just how popular “stem cell treatment” is, and how industry and many institutions offer this option.
The truth about stem cells
Unfortunately, the excitement about stem cells has outpaced the science in many areas of health care. In addition, due to ethical issues associated with the use of fetal tissue, the U.S. Food and Drug Administration has severely restricted its use. Adult stem cells have fewer regulatory issues, but the FDA has prohibited “manipulation,” which includes processing and culturing of these cells. Therefore, obtaining an abundant source of concentrated stem cells can be difficult.
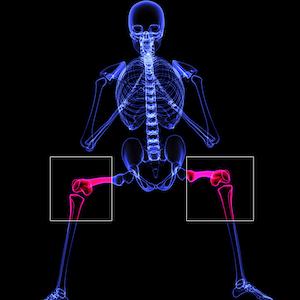
In orthopedics, researchers have proposed using stem cells for the treatment of joint – cartilage damage. This includes osteoarthritis, the thinning of cartilage that causes bones to rub against one another – similar to a car tire going bald after 50,000 miles. Osteoarthritis is the primary cause of joint replacement surgery, and stem cell injections have been promoted as a potential way to avoid joint replacement by regenerating cartilage. Unfortunately, current technology and regulatory issues make obtaining and concentrating true stem cells a challenge, and encouraging them to become and remain cartilage cells and nothing else is even more difficult.
The problem with stem cells is that these cells can continue to evolve; they may not stop development at the cartilage cell phase. They may continue to differentiate into bone cells. This would make the joint even worse because bone creates a rough surface adjacent to the smooth articular cartilage. Bone is actually the end result of arthritis.
According to the American Association of Hip and Knee Surgeons, there are no proven uses of pain medications or therapies that can delay or reverse the progressive joint destruction that occurs with osteoarthritis.
Any positive effects of current stem cell treatment are likely not the result of the actual cells themselves but something else.
Alternatives to stem cells
Separating the hype from the reality about the use of stem cells for cartilage injuries is a reminder that all patients – with advice from their doctors – need a clear picture of the potential benefits and side effects of their treatment options. This includes complications from harvesting bone marrow from the pelvis - which actually only contain less than 0.01 percent stem cells - including fracture and injury to adjacent structures and infection as detailed in The New York Times article. And while harvesting fat may seem even more attractive, the yield of actual stem cells may be even less.
Depending on the cause and severity of their knee pain, for example, patients have treatment options that range from physical therapy to injections of various medications to surgery. All have pros and cons; steroid injections can provide quick but short-lived pain relief, while a knee replacement can provide a permanent solution but also requires months of rehabilitation. Doctors need to help patients make the choice that best fits their particular needs.
So while a quick internet search may find clinics that offer stem cell treatments for cartilage injuries that cost thousands of dollars - and are almost always not covered by insurance - I strongly recommend that consumers remember the concept of “buyer beware” and that medical providers remember the Hippocratic principle: “first do no harm.”

Mark Miller, Professor of Orthopaedic Surgery, University of Virginia
This article is republished from The Conversation under a Creative Commons license. Read the original article.