“For many people, regardless of size, stepping on the scale at the doctor’s office can be a triggering, harmful experience,” SELF magazine reported late last month. “'Please don’t weigh me' cards may offer a solution.” If you're not familiar with these cards, they're sold by More-Love.org as part of an effort to change how health care providers think about the relationship between weight and health. The organization maintains that we live in “a fatphobic society” and thus
being weighed and talking about weight causes feelings of stress and shame for many people. Many people feel anxious about seeing the doctor, and will avoid going to the doctor in order to avoid the scale.
We need to address two separate issues. The first is whether or not weight is an accurate health metric; the evidence suggests that it is in many cases. The second is how health care providers communicate that information to their patients, which most of us recognize should always be done with respect. The mistake that SELF and More-Love make is minimizing the link between weight and health in order to justify changing how doctors interact with their patients. That's unnecessary at best and potentially harmful at worst.
Obesity carries health risks
As someone who struggled with obesity into my 20s, I empathize with people who fear stepping on the scale at the doctor's office. At the same time, it's clear that carrying extra weight can be detrimental to our health. A 2017 New England Journal of Medicine (NEJM) study that estimated the prevalence of overweight and obesity between 1980 and 2015 got to the heart of the matter:
"In our systematic evaluation of the health effects of high BMI, we found that excess body weight accounted for about 4 million deaths and 120 million disability-adjusted life-years worldwide in 2015. Nearly 70% of the deaths that were related to high BMI were due to cardiovascular disease, and more than 60% of those deaths occurred among obese persons."
Researchers have also documented the serious health risks associated with fat accumulation. I refer you to my colleague Dr. Chuck Dinerstein's recent, excellent piece Explaining Fat for a detailed discussion, but here are the highlights:
- Healthy white fat “exhibits extensive metabolic flexibility,” ensuring we have the energy we need.
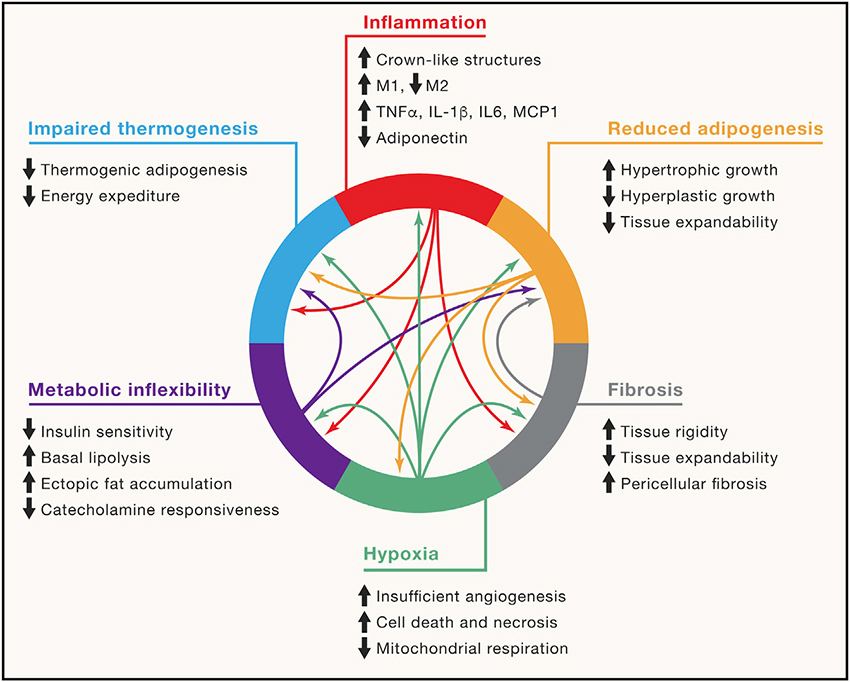
- When we take it more than we need, white fat becomes less flexible. We develop insulin resistance and make more and larger fat cells. Those cells, in turn, can cause local loss of oxygen, resulting in inflammation, fibrosis and further reducing the ability of white fat to expand in a “healthy” manner.
- When we take in less than we need, through fasting or other calorie restrictions, obesity impairs signaling, and the normal mobilization of fat to provide energy is diminished.
- “Ultimately, these pathological changes impair the critical nutrient-buffering function of adipose tissue, leading to insulin resistance and metabolic disease.”
Several qualifications could be added to this analysis. The correlation between increased BMI and mortality risk is imperfect. We know this, in part, because some studies have shown that cardiorespiratory fitness can significantly reduce the link between increased all-cause mortality and obesity.
It's also quite likely that our propensity to put on weight has a genetic component. Genome-wide association studies (GWAS) have uncovered many possible culprits lurking in our DNA. So-called “gene by environment and lifestyle interaction analyses” have also found that living in cities with fast-food joints on every corner has amplified the genetic risk of obesity for many of us. These data points support the argument that weight control isn't entirely a matter of personal responsibility, and that being overweight isn't a guarantee that you'll be unhealthy. But this doesn't settle the issue.
As the NEJM paper noted, the decoupling of obesity from conditions like cardiovascular disease may be driven in large part by a reduction in other risk factors (smoking has declined significantly in recent decades, for example) and improvements in health care. Clinical interventions “have proved to be effective in controlling high levels of systolic blood pressure, cholesterol, and fasting plasma glucose — the major risk factors for cardiovascular disease,” the authors wrote.
There is also good evidence that weight loss leads to a variety of improved health parameters, including better blood sugar, blood pressure, lipids, and mobility. Even modest weight loss can generate these results, but for some conditions, greater weight loss results in better outcomes, according to a 2020 review:
"The message to healthcare professionals is that significant improvements in health can occur with a modest weight loss of 5% while others need a larger weight loss of 10% or more. If we can obtain and sustain a weight loss of 15% or more, we are probable to produce a much greater health benefit, as well as make patients with obesity more satisfied with the outcome."
It's how you say it that matters
By failing to grapple with all this data, SELF and many other advocates of the fat-but-fit hypothesis make the same mistake many critics of vaccine mandates make: they reject sound science in order to overturn a flawed policy, or a flawed perspective in the case of weight management.
This doesn't mean the campaign against fat bias is entirely unjustified. “It says far more that a patient cannot express their feeling to their doctor and have to use a card,” Dr. Dinerstein added. “That is the ugliest sign that our healthcare relationships are broken.” In March 2020, Nature Medicine made a similar observation, publishing a “Joint international consensus statement for ending stigma of obesity.” The authors argued that “weight stigma damages health, undermines human and social rights, and is unacceptable in modern societies.” They called on their colleagues to “end weight bias."
The medical profession seems to have recognized its role in facilitating stigma against overweight patients. That's a welcome development, but it's necessary to entertain two thoughts simultaneously to get this right. We should recognize that obesity can be harmful, as the evidence clearly indicates, and that some health care providers need to treat overweight patients with more respect. Denying that the problem exists is as harmful as exaggerating it.




