
Although we are (at least temporarily) coming out of a really nasty COVID surge, don't kid yourselves. This thing isn't done with us. Experts are predicting that this could be the "end of it." Sorry, but I don't buy it. Why? Here are the number of experts who predicted in advance that a monster like the Delta variant would emerge and have started a deadly rampage around the world in mid-2021: Zero.
And here are the number of experts who predicted that omicron would set new case records that put Delta to shame: Zero

We have a virus that mutates like a madman and, despite what some experts say about this being the "end of the pandemic," I don't buy it. The segment of viral RNA responsible for the spike protein has a short attention span; Let's call it RNADHD. It is not content to make a new spike now and then. Nope, this genetic genius is the virological equivalent of the Energizer Bunny – it just keeps going.
While virologists argue (probably correctly) that viruses typically mutate to be less lethal to their hosts, this is not the problem here. The real danger is that new variants will emerge that can escape the coverage of current vaccines. In this way, emerging variants could be will be "unintentionally" more lethal rather than less.
We got a taste of this with omicron and now may be looking down the barrel of a charmer called BA.2, an omicron subvariant that seems to be even more infectious than "plain old" omicron. If the vaccines become less effective, it is even more important to have an effective therapy to control the infection – one that operates by a mechanism not involving the spike. This should ensure that the drug continues to function regardless of spike mutations. Fortunately, we have Paxlovid – a two-component drug that I've written about numerous times (1). But, like any drug, there is always a downside.
Paxlovid is really two drugs, each with a different purpose.

Figure 1. A daily dose of Paxlovid. The two peach-colored pills are nirmatrelvir, a direct-acting antiviral drug that inhibits Mpro (main protease), a critical viral enzyme needed for viral replication. The white pill is ritonavir, developed initially as an inhibitor of HIV protease. Although ritonavir was not especially useful as an HIV drug, it was found to be a potent inhibitor of cytochrome P450-3A4 (aka CYP3A4), one of the important enzymes responsible for the oxidative metabolism of drugs.

A ribbon diagram of cytochrome P450-3A4 (CYP3A4). It's pretty. Image: Wikipedia
Because ritonavir slowed the metabolism of other HIV protease drugs, allowing them to attain higher blood levels, it is referred to as a booster – a drug that doesn't actively participate in the inhibition of the target enzyme but slows the metabolism of a second drug – the actual inhibitor – allowing it to remain in the blood longer.
This is a classic example of a drug-drug interaction: one drug having an impact on the half-life or blood levels of another. Perhaps the classic example is Valium and alcohol. Although a fatal overdose of Valium is essentially impossible, when taken with alcohol, the combination can be deadly.
Ritonavir makes nirmatrelvir work better
Since nirmatrelvir is extensively metabolized by CYP3A4, its half-life is too short, and blood levels are too low to effectively inhibit COVID infection. But, if this metabolism can be inhibited, things change radically. Indeed, when nirmatrelvir is co-administered with ritonavir, its blood levels are eight times higher than for nirmatrelvir alone. This effect can be seen (assuming you have really good eyesight) in Figure 1 below.
 Figure 1. (Left) Blood levels of nirmatrelvir (alone) at different doses. The red hatched line (marked by yellow arrow) represents the EC90 (292 ng/mL) – the concentration of drug that inhibits viral replication by 90%. Note that lower doses (sorry, this is difficult to see) drop below the EC90 by 12 hours following administration, and by 24 hours, only the two highest doses cover the EC90. (Right) When administered with ritonavir, blood levels remain at or above the EC90 for days. This is why Paxlovid (ritonavir plus nirmatrelvir) is an effective drug. It reaches and stays at a blood level that is sufficient to throw a wrench into the viral replication machinery. Source: News Medical
Figure 1. (Left) Blood levels of nirmatrelvir (alone) at different doses. The red hatched line (marked by yellow arrow) represents the EC90 (292 ng/mL) – the concentration of drug that inhibits viral replication by 90%. Note that lower doses (sorry, this is difficult to see) drop below the EC90 by 12 hours following administration, and by 24 hours, only the two highest doses cover the EC90. (Right) When administered with ritonavir, blood levels remain at or above the EC90 for days. This is why Paxlovid (ritonavir plus nirmatrelvir) is an effective drug. It reaches and stays at a blood level that is sufficient to throw a wrench into the viral replication machinery. Source: News Medical
The downside: Ritonavir impacts the metabolism of other drugs.
The NIH refers physicians to the University of Liverpool drug interaction website, which lists hundreds of drugs that CYP3A4 metabolizes and how they are impacted by Paxlovid (and eight other COVID treatments (2).
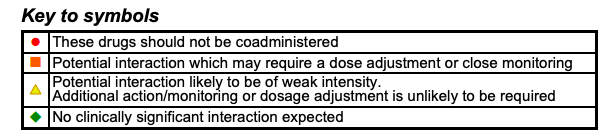
Source: Interactions with Covid-19 Antiviral Therapies
I can't possibly go through the entire list (there would be a new variant by then), but here are examples of common prescription drugs that have drug-drug interactions with Paxlovid. The degree of risk is marked as an orange circle (don't take it, period) and a red square (be careful), as well as a yellow triangle and green diamond (no worry). Here are some examples. Unless otherwise indicated, the levels of these drugs will be increased by ritonavir

- Benzodiazepines e.g., Valium, Halcion
- Statins (Zocor, Mevacor)
- Immune suppressants (Cyclosporine, Tacrolimus)
- Antidepressant (St. John's wort)
- Antiarrhythmics (Amiodarone, Flecainide)
- Misc. steroids

- Analgesics (Oxycodone (3), fentanyl)
- Antidepressants (Wellbutrin**, Tricyclics)
- Sedatives (Ambien, Xanax)
- Calcium channel blockers (Many)
- HIV medications (Many)
- Statins (Lipitor, Crestor)
** Wellbutrin (bupropion) is an outlier. Its levels (and those of its active metabolites) are lower when taken with ritonavir. Don't ask.
These lists are not comprehensive; they are designed to give you an idea of how a variety of medications are incompatible with Paxlovid because of its booster ritonavir. Pharmacists and physicians will be aware of these interactions and suspend the second drug for the five-day Paxlovid course or adjust the dose accordingly. It's a bit of a pain but well worth it.
NOTES:
(2) My apologies, but I can't help finding it hilarious that one of the drugs incompatible with Paxlovid is....ivermectin.
(3) For people who are taking oxycodone and need to take Paxlovid the recommended dose is 25% of the original dose and titrating in either direction depending on its effect on pain and side effects. Another way of saying this is that ritonavir increases oxycodone in the blood by something approximating four times.



